Positive Approaches Journal, Volume 10, Issue 4
| Site: | My ODP |
| Course: | My ODP |
| Book: | Positive Approaches Journal, Volume 10, Issue 4 |
| Printed by: | |
| Date: | Sunday, February 8, 2026, 7:39 AM |
Positive Approaches Journal | 6

Volume 10 ► Issue 4 ► February 2022
Embracing Behavioral Supports and Meaningful Applications
Introduction
If there’s one thing we’ve learned in the past year, it’s the value of being able to pivot. Our routines have been ransacked, whether we’re providing support services in our jobs or planning a family gathering. Day by day, we evaluate the risks and benefits of any activity involving an encounter with others and make choices about social distance, masks, and using hand sanitizer. The restrictions have encouraged us to develop creative ways to take part in the world around us. Meeting in parks, virtual breakout rooms, or under patio lights by a firepit is now commonplace. Flexibility once praised primarily for people in creative endeavors, has become a survival strategy. And those who have mastered the ability to adapt quickly have thrived in spite of the obstacles.
Positive Behavioral Support, when done well, merges not only evidence-based practices but also ones that are flexible and creative. All humans use behaviors that work for them. Behavior specialists work like detectives uncovering clues and solving the puzzle to determine the functions of behavior. Each plan is unique and individualized, exploring not only observable consequences but also past trauma, environment, and genetics.
Articles in this issue
encourage us to focus on merging silos of mental and physical health and
incorporating biomedical and socio-environmental influences which all play into
how a person behaves. No longer limited to practices like discrete trial
training and aprons filled with M&M’s, Positive Behavioral Support has
proven effective in a variety of messy settings where challenging behaviors are
likely to be triggered, like fast-food restaurants, playgrounds, job sites, and
people’s homes. We’ve learned that behavioral approaches, once thought to be
effective only with specific populations of people with diagnoses like autism
or intellectual disability are effective for everyone, especially when
developing plans with people who require complex mental health support. Creating
multidisciplinary teams with a variety of stakeholders who like and admire the
person needing support helps to promote a positive outcome and ensures
simplicity and ease of administering a plan that works for everyone.
If this work inspires you, check out The Home and Community Positive Behavior Support (HCPBS) Network of the Association of Positive Behavior Support. HCPBS is a nonprofit organization that is dedicated to expanding and enhancing the application of positive behavior support principles across home and community settings, contexts, and the lifespan for people with behavioral challenges (including intellectual and developmental disabilities, mental health diagnoses, and seniors who require memory care and other related services) and the systems who support them. The HCPBS website (www.hcpbs.org) is loaded with practical resources, videos, stories of people who have been helped, and a treasure trove of evidence-based practices and research.
Molly
Dellinger-Wray, MS Ed
Home
and Community Positive Behavior Support Network
Partnership
for People with Disabilities at Virginia Commonwealth University
Positive Approaches Journal | 8-12

Volume 10 ► Issue 4 ► February 2022
Data Discoveries
The goal of Data Discoveries is to present useful data using new methods and platforms that can be customized.
Positive Behavioral
Supports (PBS) include a series of strategies for supporting individuals to
improve quality of life and decrease challenging behaviors through
evidence-based methods. PBS can be used in a variety of contexts like schools,
homes, and communities.1 While often described and implemented in
disability populations like those with developmental disabilities or autism
spectrum disorder (ASD)2,2 PBS has been used
in a wide array of populations including those with childhood obesity3 and an acquired
brain injury.4,5 One of the core principles of PBS is
the Assessment of Contexts and Functions.6 Assessment is
critical in PBS to track patterns in when, how, and within what context(s) a
behavior occurs to implement appropriate supports to improve individual quality
of life. Assessments can take many forms in PBS including “…record reviews,
interviews, and observations”.6 A Functional
Behavior Assessment (FBA) is one example of a process that can gather and
measure data surrounding a behavior that is occurring and identify variables
that may be impacting the cause and effect of the behavior.7 The goal of an
FBA as part of PBS is to assess and replace challenging behaviors.
Pennsylvania, through efforts of the Office of Developmental Programs (ODP), has
been propelling strategies to support providers, across the service system and
lifespan, in execution of FBAs as well as the development of a treatment or
behavior support plan that can be used across settings through an FBA training.
The ODP FBA training has been delivered in-person and via a DVD and has
recently been upgraded to be an interactive, self-paced module online format
that is widely accessible through the MyODP web platform.
The data dashboard below shows information about PBS and FBAs from several data sources. The first tab, ‘Positive Behavioral Supports in Publications’ shows the use of PBS in various populations that have been published in academic, peer-reviewed journals through a search of scholarly journal databases for the phrase “positive behavior supports”. Click on a circle and you will be directed to the full text of the PBS articles. The size of the circle represents the number of other research articles citing that article, which is sometimes referred to as the impact of the article (e.g, the bigger the circle, the more impact or the more others have cited the article). To learn more about implementation of FBA training and practice in in Pennsylvania, click on: ‘FBA Training in Pennsylvania Over Time’ to view a timeline of training in FBA delivered in Pennsylvania by ODP FBA training. You can also learn about ‘Provider Perceptions of FBAs’ to view responses to a 2017 survey conducted by ODP and the Autism Services, Education, Resources, & Training Collaborative (ASERT) to gather opinions and perspectives about the ODP FBA training content and process. Use the filters to view responses by provider type, role function, and ages of individuals supported.
Conclusion
For more resources and training to learn more about PBS, visit the Home and Community Positive Behavior Support Network (HCPBS) website (www.hcpbs.org/). HCBPS is a clearinghouse of resources, webinars, literature, and other information focused on the application of PBS in home and community-based settings. For more information about the web based ODP FBA training, visit: https://www.myodp.org/enrol/index.php?id=1644. For more resources about FBAs from ASERT visit: https://paautism.org/resource/functional-behavioral-assessment-student-education/.
References
1. Hieneman M. Positive Behavior Support for Individuals with Behavior Challenges. Behavior Analysis in Practice. 2015;8(1):101-108. doi:10.1007/s40617-015-0051-6
2. Horner RH, Dunlap G, Koegel RL, et al. Toward a Technology of “Nonaversive” Behavioral Support. Research and Practice for Persons with Severe Disabilities. 2005;30(1):3-10. doi:10.2511/rpsd.30.1.3
3. Smith JD, St. George SM, Prado G. Family-Centered Positive Behavior Support Interventions in Early Childhood To Prevent Obesity. Child Development. 2017;88(2):427-435. doi:10.1111/cdev.12738
4. Todd A, Horner HR, Vanater S, Schneider C. Working together to make change: An example of positive behavioral support for a student with traumatic brain injury. Education & treatment of children. 1997;20(4):425.
5. Gardner RM, Bird FL, Maguire H, Carreiro R, Abenaim N. Intensive Positive Behavior Supports for Adolescents with Acquired Brain Injury. Journal of Head Trauma Rehabilitation. 2003;18(1):52-74. doi:10.1097/00001199-200301000-00007
6. What is Positive Behavior Support? Home and Community Positive Behavior Support Network (HCPBS). Accessed February 10, 2022. https://hcpbs.org/what-is-positive-behavior-support/
7. Shriver MD, Anderson CM, Proctor B. Evaluating
the Validity of Functional Behavior Assessment. School Psychology
Review. 2001;30(2):180-192. doi:10.1080/02796015.2001.12086108
Alford, Arva, Bell, Burger, Easley, Gaworski, Hollander & Treadway | 13-31

Volume 10 ► Issue 4 ► February 2022
Common Misconceptions About Behavioral Support – Debunked!
Amy Alford, M.Ed., BCBA; Heidi Arva; George Bell IV MA; Emily Burger, MS, NCC; Heather Easley; Lindsay Gaworski, M.Ed.; Jordan Hollander, M.Ed., BCBA, BSL; and Pamela Treadway, M.Ed.
Office of Developmental Programs Unified Clinical Team
Abstract
Behavioral support is often misunderstood, even while it provides a critical approach in supporting someone who may be using behaviors that interfere with optimal functioning and are challenging for supporters to understand. Applied research has provided the field with a plethora of evidence that this approach is an important consideration in treatment. The intent of this article is to provide accurate information about the behavioral approach as it applies to supporting people across the lifespan, who have varying disabilities, and work, live, and play in many settings and environments. The following misconceptions from the field will be reviewed:
- Misconception #1: Behavioral support only works for people with autism and certainly is not effective for people with mental illness.
- Misconception #2: Behavioral support is the only treatment modality that will address challenging or problematic behavior.
- Misconception #3: The more complex a person’s needs are, the more behavioral support is required.
- Misconception #4: Behavioral support is primarily focusing on developing rewards as reinforcement for the person to decrease their challenging or problematic behavior.
- Misconception #5: There is one right way to conduct a Functional Behavioral Assessment (FBA).
- Misconception #6: Behavioral support and therapy are the same.
Misconception #1: Behavioral support only works for people with autism and certainly is not effective for people with mental illness.
Research has established behavioral interventions as an effective treatment strategy for people with autism; however, that does not mean behavioral supports and interventions should be limited to those diagnosed with autism. Behavioral supports include the development and implementation of behavioral interventions that are grounded in FBA across diagnoses.
The connection between behavioral support and mental illness is often misunderstood and undervalued. Behavioral supports may be overlooked as a treatment option for people with mental illness because when we think of “behavior” we associate it with things that we can readily observe such as breaking objects, biting, or refusals to complete personal hygiene whereas mental illness is viewed as an internal or physiological state that we cannot easily observe. It is often misconstrued that there is nothing behavioral supports can do to address behavior that is attributed to an internal state. Griffiths, Gardner, and Nugent offer a comprehensive and individualized approach to functional behavioral assessment that incorporates assessment of both biomedical and socio-environmental influences.1 Biomedical factors may play a part in explaining the occurrence of problem behavior.
Behavioral assessment can effectively be utilized to understand the interaction between physiological (biomedical) and environmental factors. For example, an individual is diagnosed with an anxiety disorder and when faced with an anxiety-provoking
situation that results in physiological changes such as sweating and a pounding heart, a problem behavior such as physical aggression is triggered. An FBA can assist in identifying those situations that are associated with the physiological symptoms
of anxiety so that behavioral strategies can be put in place to prevent or reduce the likelihood of physical aggression. Additionally, the role of other biomedical factors such as medications, sleep, and medical conditions may be discovered during
the FBA which aids in the development of comprehensive behavioral interventions.
As the needs within our system grow so does the complexity of behavior. Factors like trauma, neurodevelopmental differences, environment, and genetics all play into how an individual behaves. It can create a confusing picture and many teams are not sure where to begin or what to address first. Utilizing a functional behavioral assessment can help to clarify that picture and to sort out the complexities. Mental health diagnoses are at their essence a collection of visible behaviors and internalized thoughts and emotions.2 It is not easy for the individual to sort out and verbalize nor is it easy for the outside observer. Practicing the use of purposeful, evidence-based tools allows the individual and the support team to better define and understand what is happening. Furthermore, it can potentially be determined what other factors influence the symptoms and can be changed or adapted to improve the outcome.3 There is evidence dating back to some of the very first behavior analysts that indicates that the modification of antecedents and triggers can produce different outcomes for those living with mental illness. In fact, behavior modification rooted in functional behavior assessment was used to support things like improvements in social skills, working skills, and overall independent living over 30 years ago.3
Misconception #2: Behavioral support is the only treatment modality that will address challenging or problematic behavior.
Effective behavioral supports require a multidisciplinary approach. This is especially true when the person receiving support has complex needs. Complex needs are complex because supports require a biopsychosocial approach – it’s never one thing. 3 As mentioned above, behavioral assessment can effectively be utilized to understand the interaction between physiological (biomedical) and environmental factors. Behaviors have a suspected physiological cause. It is within the scope of behavioral support to collaborate with other professionals to develop a holistic plan that includes recommendations and instructions from a multidisciplinary team, especially when the FBA does not demonstrate a clear relationship between environmental antecedent and behavioral function.
These professionals include:
- Psychiatrists for when the individual has a suspected or diagnosed condition that may require medication.
- Mental Health Professionals for when there is a suspected or diagnosed mental health condition that is outside the scope of practice for the behavioral specialist.
- Medical doctors for when there is a potential physiological cause that has been confirmed or one that has not been ruled out as a cause. A rule of thumb with a quality FBA is to rule out anything that may be medical first before developing behavioral-based strategies. This is especially important when the individual is experiencing pain, sleep issues, or food-related issues.
- Clinical Specialists such as substance abuse counselors, or sexuality specialists for when there are needs outside the behavioral specialist’s scope of competence.
Some of these professionals may already be involved when this person becomes known to the behavioral specialist and some may be identified during the FBA process when the behavioral specialists identify needs beyond their scope of practice and seek recommendations from relevant professionals. The resulting Behavioral Support Plan (BSP) should be a document that is consistent with and informed by the treatment plans developed by all members of the multidisciplinary team and is aligned with the individual’s values and goals.
Misconception #3: The more complex a person’s needs are, the more behavioral support is required.
One of the most common yet unfitting assumptions we encounter in supporting people with complex needs (i.e., needs requiring significant attention, resources, or supports) is that increases in maladaptive behavior should be met with an equivocal increase in service. In other words, the more concerning behavior a person exhibits, the more we attribute a need to increase direct behavioral supports. However, an increase in direct support is not always the answer. Of course, there are times where the challenges a person exhibits can be mitigated by increasing direct service, but often these increases can have an inverse effect, and can even exacerbate the problem. At its core, behavioral support is about the consistent implementation of the BSP by the entire support team.
As a review, let’s provide simple explanations for these two approaches.
- Direct Service: Direct implementation of strategies discussed in the BSP. These supports are often implemented by the behavior specialist, staff, family, or other caregivers and with the person themselves.
- Indirect Service: Analysis of fidelity of others implementing the plan through training, observation, data review, and feedback. Indirect services often occur without the person present, but always has the person as the focus.
In order to fully understand how to effectively support behaviors, we should first consider the philosophy of “quality over quantity.” Sometimes it is not necessarily how much direct support is provided, but rather the content, quality, and implementation of these services that truly drive effectiveness. Yet, the first response by many teams often involves some form of direct service increase. Instead of providing a quantitative response characterized by increases in direct support, emphasis should first consider a review of qualitative factors often found through indirect means. The focus should incorporate a review of plan fidelity and consistency of plan implementation. Additional indirect activities should incorporate a review of data, elicited feedback from the multidisciplinary team, observation, and additional training to supporters. It’s through these activities where most factors limiting success can be identified, resulting in a more profound impact than simply increasing direct support.
In summary, if response efforts maintain focus on indirect strategies that seek to analyze data and evaluate fidelity, changes can be made to better modify the environment and best meet the person’s individualized needs. When we question the effectiveness of supports, our focus is not always best served by increasing direct service with the individual. Instead, this provides an opportunity to enhance the implementation of indirect strategies that enable us to better understand the problem and how to best support the person. This includes an emphasis on:
- Plan Fidelity: Is the plan being implemented appropriately and consistently?
- Training: Do supporters require additional training to implement the plan more effectively and consistently?
- Data Analysis: What does the data tell us about the current situation?
- Plan
Modification: Does the data and additional analysis suggest a need to make changes to the current plan?
Adopting this approach empowers the multidisciplinary team to work collectively and ensure the application of supports is provided in a consistent manner, as they were intended, and helps to alter the practice of simply adding already ineffective direct supports as a means of better managing the person’s needs. Without these considerations, there is an increased risk of over-reliance on the behavioral specialist. After all, effective behavioral support is evidenced by empowering other members of the team to understand the function of challenging behaviors and implement individualized strategies with integrity.
Misconception #4: Behavioral support is primarily focusing on developing rewards as reinforcement for the person to decrease their challenging or problematic behavior.
When people think about behavioral support, many envision Pavlov’s dogs or Skinner’s reinforcement theory. Many think of sticker charts and token economies or tangible rewards used in discrete trials when training new skills. Though these are all components of its history, the field has grown from this simple notion of rewards and consequences to a rich tapestry of understanding and perspective rooted in the experience of the person supported.
A behavioral approach, at its core, is all about reinforcement, but the principles of reinforcement are often misunderstood. All humans engage in behavior that is functional to them. This means that our individual behavioral repertoires are developed throughout our lifetimes based on our experiences and responses to those experiences. We continue to engage in behaviors that have been successful in meeting our needs in different situations throughout our lives. Favorable consequences or outcomes make it more likely that the behavior that led to that outcome will occur in that situation in the future. This is the core of reinforcement theory, but behavioral support is so much more than a focus on decreasing challenging behavior by pairing new behaviors with rewards or privileges thought to be reinforcing.
Through the FBA process, a behavioral specialist should have a functional understanding of a person’s challenging behavior. This includes an understanding of the situations in which challenging behaviors have historically occurred as well as an understanding of WHY those situations may be challenging to the person. To understand the function is to understand the reinforcement history of that behavior. In practice, this means if the behavioral specialist has completed a quality FBA, they already know the needs of the person in specific challenging situations as well as what will likely reinforce more efficient alternative and replacement behaviors. Positive behavioral supports focus on modifying or avoiding those situations to help the person be more successful in the future. As one cannot simply suggest an environment change in isolation, one must couple that with skill-building, “...to promote performance of desired behaviors, support planners must ensure that these behaviors have been taught and that they produce adequate maintaining consequences (reinforcers) when they occur.4” This is accomplished in two ways. First teaching more efficiently achieves the same function when preventative strategies are not effective, and second, by teaching alternative behaviors that help the person cope with some of the challenges presented in those situations.
Behavior support in current practice takes a holistic approach to assessment and implementation. When a problem behavior has been identified and supports are sought, the gathering of information begins. As the assessment gives shape to the behavior support plan, we see the proactive nature of behavior support emerge. It is not about responding to a crisis and stopping the behavior at that moment but rather setting up the internal and external environment to respond proactively to avoid the crisis altogether. The plan focuses on identifying alternative, adaptive responses to a given trigger or antecedent and practicing those to create a fluidity that feels natural and then becomes the default.
Interventions focus on modeling, coaching, teaching, and transferring skills to the team and individual supported. This can only be accomplished through ongoing assessment and feedback of the efficacy of interventions and their outcomes. It
is not aversive conditioning but rather reteaching the response to triggers and antecedents and building the necessary skills to do so. Carr’s discussion suggests one can be confident that positive behavior support as an approach focuses on skill-building
and environmental design as the two vehicles for producing desirable change.5
If a person is only working for a reward when that reward is removed, the desired behavior will not likely continue. However, if you teach a person how to respond differently or adapt an environment to be more suitable, systematically fading and modifying
the reward contingencies as part of the larger plan, the conditions themselves work to change the behavior and lead to long-lasting success.
Misconception #5: There is one right way to conduct an FBA.
Behavioral support is rooted in FBA and therefore functional understanding of behavior. The FBA is not a one-time thing, but an ongoing process that should be the core of any BSP. Behavioral specialists should always base their interventions on the most current and comprehensive functional hypothesis of challenging behavior.
Unlike other assessments and tools, the FBA is an individualized process to understand why someone does what they do. By collecting information, analyzing information, and making data-based recommendations, a comprehensive BSP can be developed. If all FBAs are identical, you may be missing key information needed to understand the person you are supporting. Recognizing that an FBA is an ongoing process ensures that teams have the most up-to-date information and data to understand the function of the targeted behaviors. That being said, there are best practices to the FBA process that should be considered to ensure the BSP approaches treatment and intervention comprehensively, holistically, and individualized to the person.
The first best practice of the FBA process is through indirect and direct information gathering. Record reviews are one method of indirect information gathering which offers a historical perspective of the individual and the targeted behavior, while also gathering social, medical, educational, and/or behavioral information. There are no rules around what information must be gathered during record reviews, however, the information gathered should be relevant to the targeted behavior and understanding what may be maintaining the behaviors. Interviews are another form of indirect information gathering that offers personal perspectives from the individual and people who know them well. These personal perspectives can be gathered through questionnaires, rating tools, and/or structured/unstructured conversations. Some examples of these tools are the functional Assessment Interviews (FAI), Motivation Assessment Scale (MAS), Questions About Behavioral Function (QABF), and Functional Assessment Screening Tool (FAST). The questionnaires, tools or assessments that are used during the FBA process should provide enough information to formulate a hypothesis that will drive the multi-component behavioral support plan.
Direct information gathering includes observation of the individual in their natural environment. It should include data collection of the targeted behavior to more clearly define the behavior, support or refute the interview information, determine baseline levels and current levels of skills, provide objective information on conditions surrounding behaviors, and lead to a more accurate hypothesis of the behavior. The data collection method and items collected need to be specific to the individual. It should be succinct, targeted to the behavior of the individual, and written using clear, quantitative, consistent, and targeted language. Be sure to consider other elements of data collection beyond a frequency count (e.g. duration, latency, intensity).
Once the data is collected, a thorough analysis of the information to identify patterns, form hypothesis statements, and inform the data-based recommendations should be completed. Often, Excel or other similar programs are used to create graphs, but
there is great flexibility in how the information should be analyzed and presented to the person and other team members. The data-based recommendations should then be identified based upon the information gathered and analyzed as part of the FBA
process.
Many think this is the end of the FBA process, but this process should be ongoing for the duration of the time the person receives behavioral support. As support is provided and ongoing data is collected and analyzed, the behavioral hypothesis may
change and the strategies within the BSP must also change to reflect the most current hypothesis. The FBA must also be updated to reflect these changes.
Misconception #6: Behavioral support and therapy are the same.
The education and experience of a therapist or counselor provide an important perspective to behavioral support, but in practice it is very different from traditional therapy, counseling, or social work. Behavioral support is about more than the behavioral
specialist’s “sessions” with the individual. It is more than providing access to resources and tools. Behavioral support is more about DOING than THINKING. It uses data to assess problematic behaviors and creates a team implemented plan to teach
skills, express needs, and create more successful environments for the individual. Successful behavioral support relies primarily on the time outside the direct interaction with the behavioral specialist. Therapy, on the contrary, helps someone
develop strategies to change the way someone thinks. Primarily, a therapist works directly with the person to process feelings and emotions without direct intent to manipulate or change the environment and others in their environment.
Sometimes we feel like people need access to certain supports and when there are seemingly barriers to accessing needed supports, like counseling or therapy, the behavior specialist jumps in and takes on a role outside their scope. This well-intentioned act can be detrimental to the individual receiving services and can cross an ethical line that should not be crossed. Programs have different service lines for a reason. If someone needs therapy, they should receive therapy (in addition to behavioral support).
References
1. Gardner WI, Griffiths DM, Jo Anne Nugent, National Association For The Dually Diagnosed. Individual Centered Behavioral Interventions: A Multimodal Functional Approach. Nadd Press; 1998.
2. Wong SE. Behavior Analysis of Psychotic Disorders: Scientific Dead End or Casualty of the Mental Health Political Economy? Behavior and Social Issues. 2006;15(2):152-177. doi:10.5210/bsi.v15i2.365
3. Griffiths DM, Summers J, Chrissoula Stavrakaki. Dual Diagnosis: An Introduction to the Mental Health Needs of Persons with Developmental Disabilities. Habilitative Mental Health Resource Network; 2002.
4. Rehabilitation Research and Training Center on Positive Behavioral Support. PBS Practice. Association for Positive Behavioral Support. https://www.apbs.org/files/competingbehav_prac.pdf. Accessed January 5, 2022.
5. Carr EG, Dunlap G, Horner RH, et al. Positive Behavior Support: Evolution of an Applied Science. Journal of Positive Behavior Interventions. January 2002; 4:4-16.
Biographies
Amy Alford M.Ed., BCBA, is a Senior Clinical Consultant for the Bureau of Supports for Autism and Special Populations (BSASP), Office of Developmental Programs (ODP). She has been supporting children, adolescents, and adults with autism and other developmental disabilities for over 15 years in community, home, and school settings. She holds a master’s degree in Special Education and in 2011, became a Board-Certified Behavior Analyst (BCBA). Prior to joining the BSASP clinical team in 2008, Amy was a behavioral specialist for a provider in the Behavioral Health Rehabilitation Services (BHRS) system (now Intensive Behavioral Health Services (IBHS)). She spends much of her time leading training efforts across ODP and continues to apply principles of positive behavioral supports and applied behavioral analysis throughout her work.
Heidi Arva has worked as a Clinical Consultant for ODP’s- Bureau of Supports for Autism and Special Populations since the Spring of 2016. Prior to working at ODP, she spent over 15 years providing direct support to adults, children, and families within the mental health system.
George Bell IV, MA is is currently assigned as the Regional Clinical Director for the Northeast Region's Office of Developmental Programs, Bureau of Community Services. He has worked with the state office for seven years. Prior to his current position, he worked with a private provider agency for more than twenty years supporting individuals with intellectual and developmental disabilities in community-based programs.
Emily Burger MS, NCC is a Special Populations Professional in the Bureau of Supports for Autism and Special Populations. Prior to joining ODP, Emily worked with both the mental health and intellectual disability/autism community. She provided a wide variety of supports spanning from children's services, psychiatric rehabilitation, and residential community homes to most recently directing a behavioral support program. Currently she works with the Special Populations Unit focusing on complex cases with children, infant mental health and communication.
Heather Easley has worked for the Office of Developmental Programs (ODP)- Bureau of Supports for Autism and Special Populations as a Clinical consultant for 4 years. Prior to her work at ODP, Heather spent over 10 years supporting children, and adults across multiple systems.
Lindsay Gaworski joined ODP as a contractor in 2021 as a Clinical Director within the Western Region. Lindsay holds a Master of Education in Special Education from the University of Pittsburgh, with focused and intensive coursework in Applied Behavior Analysis. In addition, Lindsay has over 12 years of professional experience across multiple systems service lines including serving 2-5 year old children with ASD within a partial hospital setting, Intensive Behavioral Health Services (formerly BHRS) working with youth and families as a BSC while serving as a provider Autism Director, and most recently a Clinical leadership role within a residential provider. Lindsay is a graduate of the Capacity Building Institute, Year 3.
Jordan Hollander M.Ed.,
BCBA is a Senior Clinical Consultant for the Office of Developmental Programs – Bureau of Supports for Autism and Special Populations. He has been working for the past 12 years to help people on the autism spectrum identify goals, and work towards
achieving them through a person-centered approach that utilizes the principles of positive behavioral supports. Jordan has worked in various Direct Support Professional roles as well as in clinical and operational management positions for various
service providers throughout Southeastern PA.
Pamela Treadway, M.Ed., is a Senior Clinical Consultant for the Bureau of Supports for Autism Services and Special Populations, Office of Developmental Programs, Department of Human Services. She has been supporting individuals with disabilities for 42 years in home and community settings. She received a master's degree in special education from Lehigh University and has worked with adults and children with autism, intellectual disability, and emotional and behavioral disabilities.
Contact Information
Amy Alford M.Ed., BCBA
Office of Developmental Program – Bureau of Supports for Autism and Special Populations
Senior Clinical Consultant
Heidi Arva
Office of Developmental Program – Bureau of Supports for Autism and Special Populations
Clinical Consultant
c-harva@pa.gov
George Bell IV, MA
Office of Developmental Programs - Bureau of Community Supports
Clinical Director
Emily Burger MS, NCC
Office of Developmental Program – Bureau of Supports for Autism and Special Populations
Special Populations Professional
Heather Easley
Office of Developmental Program – Bureau of Supports for Autism and Special Populations
Clinical Consultant
Lindsay Gaworski
Office of Developmental Programs - Bureau of Community Supports
Clinical Director
Jordan Hollander M.Ed., BCBA
Office of Developmental Program – Bureau of Supports for Autism and Special Populations
Senior Clinical Consultant
Pamela Treadway
Office of Developmental Programs – Bureau of Supports for Autism and Special Populations
Senior Clinical Consultant
Hieneman & Fefer | 32-69

Volume 10 ► Issue 4 ► February 2022
Employing the Principles of Positive Behavior Support to Enhance Family Education and Intervention
Meme Hieneman & Sarah Fefer
I am
honored to share this article to memorialize my inspiring friend, mentor, and
colleague: Dr. Meme Hieneman. Meme lost her long and courageous battle with
cancer in August 2021. This is just one snapshot into Meme’s wide-ranging
contributions to the field of Positive Behavior Support (PBS), including
research and writing, teaching, mentoring, consulting, and advocacy work
focused on using this behavioral approach to enhance the family quality of
life. Her legacy includes many articles for Parenting Special Needs
magazine, creation of the Home and Community Positive Behavior Support Network,
development of the Practiced Routines curriculum, authoring two PBS
guides for families, leading numerous innovative and influential research
projects, and much more. I encourage you to continue to read and be inspired by
her work focused on applications of PBS in-home and community contexts.
In 2015, Meme and I co-presented at the annual conference of the Association of Positive Behavior Support to share our summary of the literature related to PBS in the context of family life. We shared models of effective family-focused intervention strategies from across disciplines and highlighted the PBS principles present in several existing evidence-based interventions for families. Our goal was to show how PBS was present in approaches that work to improve family lives. Sharing this work with fellow PBS professionals energized us to write this article to introduce the core principles of PBS to a broader range of researchers and practitioners focused on supporting individuals and families. We drew on examples of well-known family interventions to highlight their foundations in PBS principles and called for additional focus on the entire family context (rather than just on an individual or their caregivers) in future research and practice. I hope that this summary of core features of PBS will inspire others to think about how these features may be present, or how they can be enhanced, across a variety of prevention and intervention service delivery approaches in partnership with families.
Sarah A. Fefer, Ph.D. BCBA
Associate
Professor, School Psychology
University of Massachusetts Amherst
Abstract
Positive behavior
support (PBS) is an evidence-based approach for supporting adaptive behavior
and addressing behavioral challenges. It is critical that families have access
to effective evidence-based behavior support practices for both intervention
and prevention because they lead to better outcomes for families, and
counter-productive family management practices have been shown to further
escalate children’s behavioral challenges. PBS has been demonstrated to be
effective with individual children with serious behavior challenges in family
homes and features of PBS are evident in common family-based intervention
approaches. Unfortunately, complete application of PBS in family contexts has
not been fully explored or conceptualized.
The purpose of this paper is to define the core features of PBS
including lifestyle enhancement, assessment-based intervention, and
comprehensive support plans (i.e., including strategies for prevention,
teaching, and management). Examples of how the features of PBS are currently
being employed within the field of PBS and within other evidence-based parent
education and support programs are provided. Suggestions for how collaboration,
assessment, data-based decision making, comprehensive intervention, and tiered
approaches to service delivery may be used to enhance behavioral support for
families are offered. Lastly, future directions for research and practice are
recommended.
Introduction
Positive behavior support (PBS) is an evidence-based approach for supporting adaptive behavior and addressing behavioral challenges. It combines the principles of applied behavior analysis with approaches from other disciplines (e.g., ecological and community psychology, biomedical science, education) to improve the utility of behavioral intervention within typical home, school, and community environments.1,2,3,4 Although PBS was originally developed to overcome behavioral challenges of individuals with significant disabilities1, the approach has now been used successfully with a wider range of populations and applied within larger service systems (e.g., schools, mental health systems, early intervention programs, community agencies) to promote generalized behavioral improvements.5 Complete applications in family contexts, however, have been limited – even though the potential benefits are clear.
Families often experience significant stress related to child rearing, especially in dealing with children’s behavioral challenges.6,7,8 It is estimated that about 5% of children and youth experience challenging behavior9, with that figure increasing to 15% for children with disabilities.10,11 Siblings often display similar behavioral challenges12, making this a family problem. Significant behavior problems may delay children’s development, interfere with family routines, alienate children and families, and damage relationships.
When parents are knowledgeable and
skilled in effective behavioral support practices, they may use these practices
proactively, promoting family stability and creating environments in which
children thrive.13 When parents face behavioral challenges with
their children – an experience integral to family life - and do not possess the
necessary skills and knowledge to intervene effectively, they may be inclined
to resort to inconsistent, overly passive, or hostile approaches to managing
child behavior.14 Counter-productive family management practices
have been demonstrated to further escalate children’s behavioral challenges.15,16
Therefore, it is critical that parents have access to effective evidence-based
behavior support practices for both intervention and prevention.
PBS has been demonstrated to be effective with individual children with serious behavior challenges in family homes17and aspects of PBS are clearly evident in a variety of parent education programs.13, 18 It does not appear, however, that PBS has been comprehensively applied or assessed within family-based programs. In reviewing the literature, it is evident that some, but not all, features of PBS are incorporated in interventions focused on the child within the family or on the family system as a whole. In this article, we will define the core features of PBS, provide examples of how PBS is currently being employed within evidence-based parent education and support programs, and offer suggestions for how PBS may be used to enhance behavioral supports for families.
Features of Positive Behavior Support
PBS combines the technical foundations of applied behavior analysis with features derived from other fields to improve its practical utility within typical environments and routines. PBS is defined based on three core features: lifestyle enhancement, assessment-based intervention, and comprehensive support plans.1,19 Each of these features are described below with supporting literature.
Lifestyle enhancement
A foundational feature of applied behavior analysis is that the goals, interventions, and outcomes must be important and acceptable to the target individual or have “social validity”.20,21 In PBS, social validity has been interpreted as the extent to which interventions address and enhance quality of life, support teams are engaged in the process, and improvements are seen not only for individuals, but also throughout the systems that support them.
Quality of life
Quality of life refers to the extent to which an individual is satisfied and comfortable in their living circumstances.22 Quality of life is a complex multi-faceted concept that includes health and safety, self-advocacy, interpersonal relationships, productive activity, and community engagement. A critical element of life quality is self-determination – the degree to which people who are the focus of intervention efforts have a “voice and choice” in the process.23 The ultimate outcomes of PBS efforts are not only to develop skills and remediate behavior challenges, but to produce substantive improvements in lives of individuals, families, and other support and service providers.
Engagement of support teams
To ensure that PBS efforts are appropriate to the circumstances and ultimately successful, it is necessary to actively engage individuals and those who support them.24 Support teams commonly include family members, friends, neighbors, teachers, employers, therapists, social workers, and a host of other administrative and direct service professionals who may be influential in the success of PBS. The core members of these teams are included in goal identification, assessment, plan design, implementation, and evaluation.25
Support teams are engaged through planning processes that clarify desired outcomes and encompass action planning to work toward those outcomes. Various person-centered planning methods have been used within PBS.26 These planning processes guide support teams to establish a positive, unfettered vision for their future, assess available resources and potential barriers, and create a stepwise plan to work toward the goals. The limited research on the effectiveness of person-centered planning appears promising27 and its pragmatic value in PBS is evident.
Multi-tiered approach
PBS not only focuses on individuals, but also extends to the groups and systems that support them. PBS has been used extensively within schools, resulting in improvements in student attendance, academic performance, and behavior.28, 29 In addition, PBS is beginning to be employed within mental health and family support programs.30,31. These system-wide applications apply PBS principles within a multi-tiered framework in which effective behavior support practices are provided for everyone within the system proactively and universally, as well as more intensively and systematically for individuals who are at risk or experiencing significant behavioral challenges.
Assessment based intervention
Using objective data to inform and evaluate intervention is a cornerstone of PBS. It includes conducting assessments to inform strategy selection and tracking of both the integrity of implementation and outcomes of the intervention.
Assessing Contexts and Functions
PBS is grounded on the premise that effective behavioral support must be individualized based on the 1) needs of the focus individuals, 2) immediate and broader circumstances in which the individual function, and 3) consequences maintaining adaptive and maladaptive behavior patterns.32,33 It is therefore important to collect data to determine the purposes or functions behaviors are serving. Functions may include seeking attention from other people; acquiring tangible items such as food, money, games, or other desired objects; avoiding, delaying, or escaping unpleasant situations; or obtaining sensory outcomes such as increased stimulation or physical release. It is equally, if not more important, to identify the specific circumstances that set the stage for these functions.34 For example, individuals will most likely seek attention or items when deprived of them and will only endeavor to escape from situations that are uncomfortable or difficult.
Functional (and ecological) assessments in PBS involve systematically gathering information associated with the possible contexts and functions of behavior through interviews, record reviews, and observations.35,36 A variety of interview tools may be used from simple rating scales37,38,39 to more elaborate questionnaires.36 Direct observations are typically structured to obtain information on the antecedents, behaviors, and consequences40 or patterns of behavior across activities and time frames.41
Functional Behavior Assessments (FBAs) draw from multiple sources (e.g., interviewing multiple people, observing across settings and situations). Once sufficient data are collected, patterns of behavior are summarized in hypothesis statements. These statements describe the behaviors of concern, the circumstances in which they are most and least likely to occur, and the consequences that reliably follow the behavior (namely, their functions). For example, a hypothesis might be: “When Louis is asked to complete a difficult chore and not provided with frequent supervision, he will ‘get into stuff’ (e.g., take apart items or construct games). This delays completing the task and results in his parents increasing their guidance and attention.” These statements reflect the ‘best guess’ of the patterns but must be supported by data to be validated. That is done by either testing the hypotheses by manipulating events surrounding the behavior or implementing interventions based on them and evaluating their outcomes.42,43
Data-based decision making
Objective data are used to assess both the fidelity with which strategies are employed and the outcomes of intervention. These data guide decision-making and determine the need for adjustments to strategies and supports.44,45 For plans to be effective, they must be implemented as designed and with consistency. Therefore, a key feature of PBS intervention is to establish systems (e.g., checklists, periodic observations of strategy use) to ensure fidelity in practice.46 The data on behavior patterns may also offer insight into whether strategies are used successfully since variations in frequency/intensity can indicate that plans are not being used as intended under every circumstance.
Data are collected on behaviors that are most important and/or the best indicators of progress. These data may include discrete measures (e.g., frequency, duration) of particular behaviors that are a focus of intervention. The behaviors measured may include those targeted for increase such as appropriate communication (e.g., using words rather than physical aggression), independent participation in daily activities (e.g., household chores, work or school, self-care), or use of particular coping strategies. They may also include behaviors individuals need to decrease to be successful or safe including, for example, yelling at or threatening other people, stealing, or engaging in behavior that disrupts valued routines.
In addition to these more narrowly
defined behaviors, PBS also assesses quality of life outcomes as described
above).5 As a result of intervention, data should capture whether
people are able to go more places, do more things, and gain more enjoyment and
satisfaction from their daily lives.47
Since PBS is implemented in complex community settings (vs. segregated or controlled environments) and within natural routines, measures often need to be adapted to improve their ease of use for individuals and their caregivers. PBS practitioners therefore often supplement or replace the direct observation or continuous recording procedures commonly used in ABA with rating scales and sampling practices.44 By doing so, the rigor may be reduced, but contextual fit and fidelity of implementation are typically increased.
Comprehensive Intervention
Interventions in PBS are directly linked to the patterns identified in the assessment. They include immediate antecedent and consequence interventions, as well as broad lifestyle changes to support the more discrete strategies. A useful framework for selecting appropriate strategies is the competing behavior model.36Using this model, we identify interventions that are logically associated with particular patterns.
Components of PBS
PBS interventions are not stand-alone procedures, but include a combination of proactive, teaching, and management elements. These elements are described briefly in the following sections.
Proactive strategies include environmental and social arrangements that prompt positive behavior and make engagement in problem behavior unnecessary by modifying or removing the triggering stimuli.49 Examples of proactive strategies include: noncontingent access to attention, tangibles, and other reinforcers50; offering choices between items or activities51; activity scheduling to prepare for upcoming events52; and curricular modifications such as embedding easy or interesting features or reducing length or difficulty of tasks.53, 54
Teaching skills includes direct instruction in two types of competencies: (a) replacement behaviors and (b) other desired skills. Replacement behaviors are more appropriate responses that meet the same function as behaviors of concern. Functional communication training, for example, is a well-documented approach in which individuals are instructed to use words or other methods of expression to ask for items, attention, or breaks, depending on the purpose or function of the behavior.55, 56 More complex skills such as negotiation and problem-solving may also be taught as replacement behaviors. Other desired skills allow individuals to participate successfully in typical daily routines and meet the expectations of their circumstances. These may include social (e.g., engaging in conversations, playing games) and daily living (e.g., completing chores, homework, or other tasks) skills.57
Managing consequences involves maximizing reinforcement for positive behavior and reducing or eliminating reinforcement for problem behavior.58, 59, 60 To manage consequences effectively, the function of the behavior – access to attention or items/activities, escape, or sensory outcomes - must be clear and access to the specific reinforcers controlled. For example, consequences may involve delivering high rates of attention or reducing demands when individuals are cooperative, but not when they are complaining or aggressive.
Implementing PBS plans
Proactive, teaching, and management strategies are combined into comprehensive PBS plans that are tailored to the circumstances. These plans should be in writing and include goals and behaviors of concern, a summary of the patterns affecting behavior, descriptions of strategies and how they will be employed across situations, and methods for monitoring outcomes. For example, if a person’s behavior is motivated by attention from peers and the goal is to improve relationships, the plan might include creating opportunities for appropriate interactions (e.g., scheduling supervised gatherings, joining clubs, setting aside time for 1:1 interaction), teaching the individual any communication or social skills needed to obtain attention, and encouraging peers to respond to conversational turn taking instead of name-calling or threats. The individual could track the frequency of his or her interactions with other people and, together with peers, rate their quality.
In addition to these immediate strategies, other supports focused on setting events are often included as well. This means not only focusing on remediating behavioral challenges, but on creating universal, proactive measures to support positive behavior. Examples of these type of supports include restructuring routines or settings to better match people’s needs, rebuilding damaged relationships to improve the overall quality of interactions, addressing health or safety concerns that may be affecting behavior, or simply finding ways to offer more choice and personal autonomy.
As the PBS plan is being finalized, it is critical to consider its contextual fit given the people, settings, and systems that will be influenced by the plan.61 Questions to guide this consideration include: Is the plan right for the individual(s) for whom it is designed (i.e., given their characteristics, needs, abilities, preferences, and motivations)? Is the plan feasible given the resources available and doable within typical routines and settings? Do caregivers and others involved in supporting the plan have buy-in and the capacity to implement? Are broader systems (e.g., home, school, work, community) aligned with the plan and therefore likely to enhance sustainability62? Responses to these questions determine whether a plan needs to be adapted or whether accommodations may be needed.
Developing an action plan that addresses
the considerations above and spells out how each aspect of the plan will be put
in place is important to support implementation.44 The action plan
includes what exactly needs to be done, who will do it, and when it will be
completed. Action items typically include rearranging environments,
establishing routines, obtaining resources, providing training and coaching,
and establishing systems for monitoring implementation and outcomes and
communicating about progress. In addition, action planning often includes ways
to support and motivate plan implementers (e.g., via reminders, tools,
incentives).
A key to ensuring that PBS plans will be implemented
consistently and effectively is to embed strategies within typical daily
routines.63 Doing so reduces the demands on implementers and
increases sustainability as the strategies become part and parcel of routines
themselves. Examples of target routines may include tasks (e.g., chores,
homework, work responsibilities), personal care, play or leisure activities,
errands, and community outings. Effective instructional practices that are
inherent in the features of PBS may be used without disruption. These include
defining specific skills to teach; arranging settings to promote independence
and success; modeling, prompting, and shaping behavior; and using differential
reinforcement to establish and maintain skills over time.
EXAMPLES OF APPLICATION OF PBS FEATURES IN FAMILY INTERVENTION
Many well-established family education and support programs include features that are consistent with those that characterize PBS. In this section, we will highlight some examples, and demonstrate that, although comprehensive family-based PBS is not commonplace, current approaches do embrace these principles. The goal is not to provide an exhaustive review of all possible programs, but to share illustrations from the field of PBS and broader family intervention approaches.
Lifestyle Enhancement
Quality of life
Both researchers and practitioners have emphasized the importance of focusing on lifestyle enhancement when supporting behavior in family contexts. While few examples of direct quality of life measurement at the family level are available, Smith-Bird and Turnbull64 demonstrate that the intervention approaches and outcomes reported in past research on family focused PBS align with the key domains of the Beach Center Family Quality of Life Scale. Three themes related to quality of life were found in their analysis of past family PBS research: a focus on daily routines that are valued by families, improved family interaction, and increased safety/physical well-being for all family members.
Examples of routines that have been addressed in family-based PBS research include dinner, play, cleanup, bedtime, bathroom, or grocery shopping, or eating at a fast-food restaurant65, 66,67 also demonstrate ongoing direct measurement of individual quality of life through a community activity inventory. More comprehensive application and measurement of quality of life within family contexts in PBS is surprisingly limited.
Beyond literature in PBS, several evidence-based programs focus on empowering families to determine desired outcomes that will benefit their overall lifestyle. For example, the continuum of interventions offered within the Positive Parenting Program68 provides choices for families and promotes self-determination, while the Family Check-Up (FCU) program capitalizes on parent motivation by providing a menu of intervention options to families after an initial assessment and feedback session.69 Meta-analytic research suggests that involving parents in generating solutions is associated with higher ratings of satisfaction, self-efficacy, and social support.70
Comprehensive family intervention programs also directly measure outcomes associated with family quality of life. The Multidimensional Foster Care program71 measures quality of life through parent report, and targets other child and parent resiliency outcomes including interpersonal relationships, stability in home context, and social support.72 PPP has been shown to enhance parent and child well-being and parent relationship quality73, and FCU led to increased parental perceptions of social support and relationship satisfaction, decreased parenting stress, and fewer child challenging behaviors.74 The Incredible Years programs, which target increasing the family support network, have been shown to increase positive family communication and parental self-confidence, and reduce parental depression.18
Engagement of support teams
Given the focus on enhancing quality of life, it naturally follows that programs supporting families would endeavor to engage people across different systems and settings. This objective is explicit in wraparound76, 77 and group action planning77, both of which have been combined with PBS. The wraparound process, like PBS, involves a team of individuals working together to develop supports to enhance the life of individuals with disabilities across multiple important life domains.79 Group action planning expands on person-centered planning practices commonly used in PBS and is also directed by the preferences of an individual and their family.77 These approaches focus on coordinating supports by engaging all relevant family members and service providers in assessment, planning, and implementation to remediate challenges.
Coordinating multiple service providers is also common within other family-centered intervention programs beyond PBS, such as MTFC, in which weekly meetings are held with the family, clinicians, therapists, and skills coaches to review progress and engage in treatment planning.80 The FCU program also includes an “ecological management” option on the intervention menu for families who would benefit from coordination of the intervention with other child and family-focused community services.69 Family and support team involvement in intervention planning, and the measurement of outcomes associated with positive child and parent lifestyle change, are primary themes across a broad range of evidence-based family focused interventions.
Multi-tiered approach
Multi-tiered service delivery can be used within systems that provide support to multiple families to ensure that the level of service provided is aligned with the need demonstrated by the family. Several research teams have proposed the application of a multitier framework to enhance the efficiency of family-engagement practices in early childhood settings31, family support in urban family service agencies31, and parent training for young children with developmental disabilities.81 Tier 1 includes low intensity strategies available for all families such as reading materials about positive parenting strategies81, 82, parent workshops, or parent-teacher conferences Tier 2 involves more intensive group-based parent training or facilitated problem-solving sessions.31,80, 82, Tier 3 includes individualized supports for families with more persistent and intensive needs such as home-based sessions with video feedback80, structured reading or home-visit programs80, or direct training.31 The model empirically evaluated by Phaneuf and McIntyre82, but not frequently utilized in practice, is based on response to intervention logic, with all families starting with tier 1 supports.
PPP is a well-researched example of a multi-tiered model of family support.83 Triple P or PPP includes five levels or tiers starting with universal communication strategies such as posters or billboards, tv or radio commercials, or brochures. The aim of this level of support is to reach all families to share parenting strategies and de-stigmatize asking for help.84 The second level of support involves brief parent support during a routine pediatrician visits, followed by level 3 which includes repeat brief and specific consultation about child behavior. Level 4 is intensive group-based training in positive parenting skills, and level 5 is an individualized Enhanced Triple P program.84 This model of parent training is unique in that it acknowledges the unique needs of families, embeds family support within the broader societal context by implementing universal campaigns to put parenting on the public agenda, and draws upon existing services within the community.84 These aspects likely contribute to PPP being one of the most widely adopted models of parent training internationally.
The Incredible
Years programs also use multi-tier logic in acknowledging that children
present with various needs which may be targeted through varying levels of
direct intervention with children, teachers, or parents, or through more
comprehensive combined approaches.84 Within this conceptualization
of the tiered model less intensive supports are viewed as those that focus on
the child or parent alone, rather than intervening at the level of the family
system by working with both children and parents to reduce challenging
behavior. Webster-Stratton and Hammond85 demonstrated that working
with both children and parents (versus child
or parent-focused intervention) produced more positive and sustainable
outcomes; however, the authors acknowledged that this comprehensive approach
may not be needed by all families. The effectiveness of this more intensive
combined approach has also been demonstrated by Parent-Child Interaction Therapy.87
Assessment-Based Intervention
Assessment of contexts and functions
Collaboration between providers and families to complete functional assessments (e.g., interviews, observations, rating scales) and inform routine-based functional interventions is common within family-based PBS.88 Several research teams emphasize partnering with family members during this assessment process or supporting family members to carry out comprehensive functional assessment processes within family homes and during natural routines.89, 90, 91 This process often involves families identifying the most problematic routines for their child to serve as the context for the implementation of PBS, as well as the identification of prioritized target behaviors.65, 66, 92, 93, , Moes and Frea63 demonstrate that directly interviewing parents to gather information about the family context (e.g., routines, goals, supports, demands) can enhance the effectiveness of family-centered interventions such as Functional Communication Training.
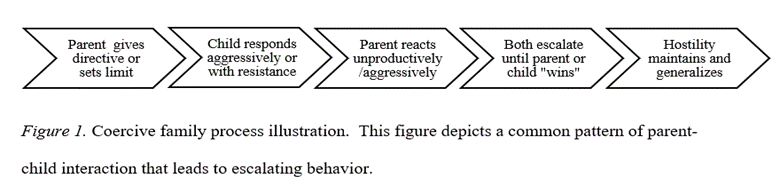
Preliminary work by Lucyshyn and colleagues94 also suggests that clinicians should directly assess parent-child interactions to determine patterns of reinforcement between parent and child that may escalate problem behavior. A possible reciprocal interaction between parent and child behavior is depicted in an illustration of the coercive family process in Figure 195 in which child behavior prompts unproductive parental responses, which thereby escalate child behavior. Using this perspective, the child’s behavior within the family context is of interest, along with the parent and child reactions that perpetuate those patterns and reinforce continuation of parental behavior.
This reciprocal or transactional relationship between parent and child behavior is the premise of many family-focused intervention programs that teach parents how to change their responses to their child’s behavior to prevent further escalation. PCIT96 involves direct observation of parents and children together, which informs the use of in-the-moment coaching for parents to improve their interactions and reduce coercive processes.97 The FCU program also includes observations of parents and children interacting in the home setting as part of a comprehensive assessment, which is used to inform a parent feedback session using motivational interviewing techniques to support parents in their choice of interventions from a menu of treatment options.69
Data-based decision making
The examples of family-based PBS research highlighted in the previous section incorporate multiple systems of data collection including structured observations and standard recording forms to look at the frequency, duration, and intensity of positive and challenging behaviors.66 These often include intensive direct observation and/or videotaping by the researchers themselves.
Although it would seem essential to engage families in monitoring progress (e.g., in order to capture data across situations throughout the day), there are fewer examples of direct parent involvement in this type of data collection for ongoing decision making.88,98, Few studies of family-focused PBS report treatment fidelity data, and those that do tend to use videotaped sessions to complete fidelity checklists rather than involving parents in monitoring their strategy use92, probably due to limitations in translating this type of intensive data collection from research to practice in family contexts. Lucyshyn and colleagues66, however, provide a comprehensive example of ongoing data-based decision making in partnership with families by including parent reports of problem behaviors as one source of information to monitor progress and make decisions to alter the intervention.
Family intervention programs beyond PBS provide
other examples of data-based decision making within the family context. PPP programs include tracking of the
fidelity of training components83 and methods to engage parents in
ongoing data-based decision making by teaching independent problem-solving
skills and providing tools and strategies to self-monitor the use of specific
skills taught.13 The most intensive individualized version of PPP, known as Enhanced Triple P, uses assessment data to guide individualization
of specific parent training modules based on family needs.83 PCIT87and Parent Management Training99
both use direct and indirect reports of interactions between children and
parents to guide the specific components of treatment and to evaluate progress.
PCIT uses data to inform the length
of the intervention; the intervention ends when parents master targeted
parenting skills and report that they are confident in managing child behavior.87
Comprehensive Interventions
In PBS, interventions are based on assessments and there is some degree of consistency in applying the framework that includes proactive and preventive strategies to address setting events and antecedents that precede behavioral patterns; teaching of desired and replacement skills; and reinforcement for positive, not problem, behavior in family contexts. Duda and colleagues65, for example, demonstrate that a combination of prevention, instruction, and reinforcement strategies reduced challenging behaviors across multiple home routines (e.g., play, cleanup, dinner). The strategies include social stories, providing choices, increasing proximity to the parent, pre-teaching rules, modeling and prompting appropriate play behaviors, teaching self-monitoring, a reward choice menu, and parent attention and praise. Lucyshyn et al.66 use similar prevent-teach-manage strategies, as well as information about family ecology to improve the contextual fit of the behavior support plan. Contextualized programs using family information (such as caregiving demands, family support needs, and social interactions goals) within comprehensive intervention programs are shown to be more effective at increasing replacement behaviors and decreasing challenging behaviors100 and lead to greater sustainability of communication skills.63
Pivotal Response Training101 also incorporates the three elements of comprehensive behavioral support, with an emphasis on teaching parents to use specific prevention (e.g., increasing child motivation through choice), teaching (e.g., modeling of new skills to encourage communication), and reinforcement (e.g., responding to all approximations of behavior with natural reinforcers) strategies within everyday activities and on an ongoing basis to increase skill development. These components are the basis for other intervention programs such as Prevent-Teach-Reinforce.102 Recent studies show that comprehensive intervention plans developed using the PTR model are effective to decrease challenging behavior and increase alternative behavior in young children and demonstrate that parents can effectively implement and generalize this intervention approach within family routines.103, 104 These PBS components have been integrated into other research as well. For example, Durand and colleagues17demonstrate the effectiveness of combining these core components of PBS with a cognitive behavioral therapy intervention to promote parental optimism.
Kazdin’s99 Parent Management Training is a forerunner in translating
behavioral principles into a comprehensive intervention approach for families.
Parents are taught specific behavioral strategies relevant to teaching and behavior
management such as praise, planned ignoring, time-out, and shaping within the
home context. Incredible Years, PCIT,
Triple P, and Multisystem Treatment
Foster Care follow suit and incorporate features of comprehensive behavior
support, as well as focus on preventing the coercive cycle. This is
accomplished in these programs by teaching parents’ prevention strategies
(e.g., increased praise and decreased criticism/commands, limit setting,
supervision/monitoring, relationship building), methods to model and prompt new
skills and positive behaviors, and specific reinforcement (e.g., structured
token economy system, increased attention to positive behavior and decreased
attention to negative behavior). A recent randomized clinical trial also
demonstrates the effectiveness of parent training that includes prevention,
teaching, and management strategies.105
Programs with Multiple PBS Components
Several books have
been written for professionals and parents specifically about parenting and
positive behavior support, combining these different features. They include
resources for professionals and parents. The first known resource related to
family PBS was Families and Positive
Behavior Support106, which included practical applications of
principles, case studies, and preliminary research in family contexts.
Hieneman, Childs, and Sergay107 made this information accessible for
parents in a self-guided problem-solving workbook that also offers suggestions
for universal supports. Durand and
Hieneman108 outlined a similar process for professionals working
with families entitled Positive Family
Intervention (that also includes cognitive-behavioral strategies to
overcome parental pessimism as a barrier to implementation). Durand109
wrote Optimistic Parenting to make these
approaches accessible to parents and added components of mindfulness and family
social support. Finally, as mentioned
earlier, Dunlap and colleagues102 have produced a Prevent-Teach-Reinforce for Families
manual written for practitioners working with families that outlines
comprehensive assessment and contextualized intervention approaches for home
and community settings.
RECOMMENDATIONS FOR PRACTICE
Over the years, ongoing research and field-based intervention with families has led to an increasing number of evidence-based clinical practices110. The way in which those practices are organized, selected, and delivered may be informed by both the principles of PBS and the growing body of literature on effective family support approaches. We offer the following recommendations based on this review:
Quality of life outcomes
Ensure that the goals of intervention are focused on quality-of-life improvements and fully embraced by the family – that they have social validity and contextual fit. Align goals with the families’ strengths, resources, needs, priorities, preferences, supports, and stressors. This means guiding, rather than directing, goal selection via processes of person and family-centered planning.
Family engagement
Engage all relevant family members and others whose involvement could influence the outcomes, valuing their input and rights as decision makers. Ensure their involvement in all aspects of the process of goal identification, assessment, plan design, implementation, and evaluation. Empower families to apply the principles (rather than just procedures) of PBS and become collaborative problem-solvers.
Comprehensive assessment
Conduct structured, comprehensive assessments to develop a valid understanding of immediate patterns and broader ecological variables affecting behavior within the family. Use the coercive family process95 framework to help families understand reciprocal interactions that may be maintaining problem behavior. Develop and utilize assessment tools36 to effectively and efficiently capture variables precipitating and maintaining behavior within families.
Support strategies and interventions
Develop support strategies and interventions based on the assessments that are truly individualized to children, parents, families, and the contexts in which they live. Use the patterns identified and the categories of proactive, teaching, and management strategies to scaffold plan design and as framework for selecting services. Help families select relevant, evidence-based strategies that fit their needs (rather than simply adopting programs or procedures to which they are exposed), encouraging individualized, creative solutions that are aligned with families’ goals, values, and culture.
Monitoring fidelity and outcomes
Rely on objective information to assess the fidelity of plan implementation, increases in desirable behavior, decreases in problem behavior, and changes in quality of life. In addition to using clinical judgment and standardized tools, create and use behavioral anchors to structure observations and interviews. Engage parents in evaluating progress, combining simple subjective ratings and feasible recording procedures to capture of specific, meaningful outcomes. Focus data collection not only on child behavior or parental skills, but also overall family functioning.
Tiered programs
Embrace the ecological multi-tiered
conceptualization of intervention. Recognize that supports may be focused on
the child within the family system, parent as a conduit for change, family as a
whole, and/or broader support systems. Establish tiered programs that offer information
and resources on PBS to all families, more tailored supports for those at risk
or struggling, and intensive individualized assistance for those with the most
significant challenges. Develop methods for “triaging” families, assessing
their response to intervention, and transitioning within a continuum of
services.
FUTURE DIRECTIONS
Positive behavior support offers a useful framework for selecting, integrating, and evaluating evidence-based behavior support practices. The focus on lifestyle enhancement and engagement of support and service providers increases the likelihood that interventions will be readily adopted and sustainable. Comprehensive assessments of both contextual issues affecting behavior and functions maintaining interactions among family members allows the tailoring of strategies to family needs, thereby increasing their effectiveness. Finally, employing proactive, teaching, and management strategies within typical family routines offers a conceptually sound and easily adoptable approach.
These features are evident in family-based intervention both within the PBS literature and broader parent education and support programs. What appears to be missing is a comprehensive, integrated model of service delivery that embraces all features equally. This gap may, in part, be due to a few barriers. First, families whose children may be having behavioral challenges have often been viewed as the problem, or as recipient of services, rather than true partners.111 Current best practice in behavioral intervention and family support emphasizes respect for the strengths, resources, needs, priorities, and perspectives of all participants, with interventionists embracing a more facilitative role.112 Unfortunately, these values are not always evident in practice.
Second, professionals from different disciplines have often worked within their own theoretical and pragmatic “silos”, making fusion of knowledge and practices challenging.113 To bring about lifestyle change, PBS often requires the integration of a variety of services and supports, but it has not always been clear how to make this integration feasible. Wraparound process and strengthening systems of care75, 79, must therefore become a fundamental part of behavior support within family contexts.
Third, families who need support most are often stressed and discouraged, making them less responsive to education and intervention.114 This barrier has been addressed through ‘adjunctive supports’ such as respite, social support, and additional therapies in parenting programs.115 More recently, cognitive behavior therapy techniques such as optimism training17, 108, mindfulness practice116, and related interventions such as Acceptance and Commitment Therapy117 and Cognitive Behavioral Family Intervention118 have been more fully embedded within behavioral intervention with families. These approaches not only address behaviors of concern, but help parents overcome emotional barriers to implementation of the plans.
And finally, PBS and other comprehensive interventions may be viewed as highly complex and time-consuming, driven by intensive data collection and circumscribed procedures that may seem difficult to implement fully.119 To be acceptable and feasibly adopted, PBS’s core components must be distilled and packaged within user-friendly resources that are readily accessible to families and professionals supporting them (see examples of brief resources on apbs.org-families). Progress is clearly being made in integrating PBS features into family-based behavior support, but more work needs to be done to bring a comprehensive approach to complete fruition.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
References
1. Carr EG, Dunlap G, Horner RH, et al. Positive Behavior Support. Journal of Positive Behavior Interventions. 2002;4(1):4-16. doi:10.1177/109830070200400102
2. Dunlap, G. Sailor, W., Horner, R. H., & Sugai, G. (2009). Overview and history of positive behavior support. In W. Sailor, G. Dunlap, G. Sugai, & R. Horner (Eds.), Handbook of positive behavior support (pp. 3-16). New York: Springer.
3. Horner RH, Dunlap G, Koegel RL, et al. Toward a Technology of “Nonaversive” Behavioral Support. Journal of the Association for Persons with Severe Handicaps. 1990;15(3):125-132. doi:10.1177/154079699001500301
4. Kincaid D, Dunlap G, Kern L, et al. Positive Behavior Support. Journal of Positive Behavior Interventions. 2015;18(2):69-73. doi:10.1177/1098300715604826
5. Lucyshyn,, J. M., Dunlap, G., & Freeman R.(2015). A historical perspective on the evolution of positive behavior support as a science-based discipline. In F. Brown, J. Anderson, & R. De Pry (Eds.), Individual positive behavior supports: A standards-based guide to practices in schools and community-based settings (pp.3-25). Baltimore, MD: Paul H. Brookes Publishing.
6. Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research. 2006;50(3):172-183. doi:10.1111/j.1365-2788.2005.00732.x
7. Neece CL, Green SA, Baker BL. Parenting Stress and Child Behavior Problems: A Transactional Relationship Across Time. American Journal on Intellectual and Developmental Disabilities. 2012;117(1):48-66. doi:10.1352/1944-7558-117.1.48
8. Spratt EG, Saylor CF, Macias MM. Assessing parenting stress in multiple samples of children with special needs (CSN). Families, Systems, & Health. 2007;25(4):435-449. doi:10.1037/1091-7527.25.4.435
9. Pastor, P.N., Rueben, C.A., & Duran, C.R. (2012). Identifying emotional and behavioral problems in children aged 4-17 years: United States, 2001-2007. National Health Statistics Reports, 48, 1-18.
10. Einfeld SL, Tonge BJ. Population prevalence of psychopathology in children and adolescents with intellectual disability: II epidemiological findings. Journal of Intellectual Disability Research. 2007;40(2):99-109. doi:10.1046/j.1365-2788.1996.768768.x
11. Lowe K, Jones E, Allen D, et al. Staff Training in Positive Behaviour Support: Impact on Attitudes and Knowledge. Journal of Applied Research in Intellectual Disabilities. 2007;20(1):30-40. doi:10.1111/j.1468-3148.2006.00337.x
12. Alexander JF, Robbins MS, Sexton TL. The Journal of Primary Prevention. 2000;21(2):185-205. doi:10.1023/a:1007031219209
13. Sanders MR, Turner KMT, Markie-Dadds C. Prevention Science. 2002;3(3):173-189. doi:10.1023/a:1019942516231
14. E Mark Cummings, Davies P. Children and Marital Conflict : An Impact of Family Dispute and Resolution. Guilford; 1994.
15. Burke JD, Pardini DA, Loeber R. Reciprocal Relationships Between Parenting Behavior and Disruptive Psychopathology from Childhood Through Adolescence. Journal of Abnormal Child Psychology. 2008;36(5):679-692. doi:10.1007/s10802-008-9219-7
16. Chamberlain P, & Patterson, GR. (1995). Discipline and child compliance. In M. H. Bornstein (Ed.), Handbook of parenting: Applied and practical parenting (Vol. 4; pp. 205– 225). Mahwah, NJ: Erlbaum.
17. Durand VM, Hieneman M, Clarke S, Wang M, Rinaldi ML. Positive Family Intervention for Severe Challenging Behavior I. Journal of Positive Behavior Interventions. 2012;15(3):133-143. doi:10.1177/1098300712458324
18. Webster-Stratton C, Reid MJ. Treating Conduct Problems and Strengthening Social and Emotional Competence in Young Children. Journal of Emotional and Behavioral Disorders. 2003;11(3):130-143. doi:10.1177/10634266030110030101
19. Horner RH, Carr EG. Behavioral Support for Students with Severe Disabilities. The Journal of Special Education. 1997;31(1):84-104. doi:10.1177/002246699703100108
20. Schwartz IS, Baer DM. Social validity assessments: is current practice state of the art? Journal of Applied Behavior Analysis. 1991;24(2):189-204. doi:10.1901/jaba.1991.24-189
21. Wolf MM. Social validity: the case for subjective measurement or how applied behavior analysis is finding its heart1. Journal of Applied Behavior Analysis. 1978;11(2):203-214. doi:10.1901/jaba.1978.11-203
22. Schalock RL. The concept of quality of life: what we know and do not know. Journal of Intellectual Disability Research. 2004;48(3):203-216. doi:10.1111/j.1365-2788.2003.00558.x
23. Wehmeyer ML (2015). Strategies to promote self-determination. In F. Brown, J. L. Anderson, De Pry, R. L. (Eds.), Individual positive behavior supports: A standards-based guide to practices in school and community settings (pp. 319-332). Baltimore, MD: Paul H. Brookes Publishing.
24. Benazzi L, Horner RH, Good RH. Effects of Behavior Support Team Composition on the Technical Adequacy and Contextual Fit of Behavior Support Plans. The Journal of Special Education. 2006;40(3):160-170. doi:10.1177/00224669060400030401
25. Bambara LM. & Kunsch C. (2014). Effective teaming for positive behavior support. In F. Brown, J. Anderson, & R. De Pry (Eds.). Individual positive behavior supports: A standards-based guide to practices in school and community-based settings (pp. 47-70). Baltimore: Paul H. Brookes.
26. Kincaid D. & Fox L. (2002). Person-centered planning and positive behavior support. In S. Holburn & P. Vietze (Eds.), Person-centered planning: Research, practice, and future directions (pp. 29-49). Baltimore, MD: Paul H. Brookes Publishing.
27. Claes C, Van Hove G, Vandevelde S, van Loon J, Schalock RL. Person-Centered Planning: Analysis of Research and Effectiveness. Intellectual and Developmental Disabilities. 2010;48(6):432-453. doi:10.1352/1934-9556-48.6.432
28. Bradshaw CP, Mitchell MM, Leaf PJ. Examining the Effects of Schoolwide Positive Behavioral Interventions and Supports on Student Outcomes. Journal of Positive Behavior Interventions. 2009;12(3):133-148. doi:10.1177/1098300709334798
29. Horner RH, Sugai G, Smolkowski K, et al. A Randomized, Wait-List Controlled Effectiveness Trial Assessing School-Wide Positive Behavior Support in Elementary Schools. Journal of Positive Behavior Interventions. 2009;11(3):133-144. doi:10.1177/1098300709332067
30. Duchnowski, AJ, & Kutash K. (2009). Integrating PBS, mental health services, and family- driven care. In W. Sailor, G. Dunlap, G. Sugai, & R. Horner (Eds.), Handbook of positive behavior support (pp. 203-231). New York, NY: Springer.
31. McCart, A, Wolf N, Sweeney HM, Markey U, & Markey D J. (2009). Families facing extraordinary challenges in urban communities: Systems-level application of positive behavior support. In W. Sailor, G. Dunlap, G. Sugai, & R. Horner (Eds), Handbook of positive behavior support (pp. 257-277). New York, NY: Springer.
32. O’Neill RE, Hawken LS, & Burdock K. (2015). Conducting functional behavioral assessments. In F. Brown, J. L. Anderson, De Pry, R. L. (Eds.), Individual positive behavior supports: A standards-based guide to practices in school and community settings (pp. 259-278). Baltimore, MD: Paul H. Brookes.
33. Wacker, DP, Berg WK. Harding JW, & Cooper-Brown LJ. (2011). Functional and structural approaches to behavioral assessment of problem behavior. In W. W. Fisher, C. C. Piazza & H. S. Roane (Eds.), Handbook of applied behavior analysis (pp. 165-181). New York, NY: Guilford Press.
34. Stichter JP, Hudson S, Sasso GM. The Use of Structural Analysis to Identify Setting Events in Applied Settings for Students With Emotional/Behavioral Disorders. Behavioral Disorders. 2005;30(4):403-420. http://www.jstor.org/stable/23889852
35. Anderson CM, Long ES. Use of a structured descriptive assessment methodology to identify variables affecting problem behavior. Journal of Applied Behavior Analysis. 2002;35(2):137-154. doi:10.1901/jaba.2002.35-137
36. O’Neill RE, Albin RW, Storey K., Horner RH, & Sprague JR. (2015). Functional assessment and program development for problem behavior: A practical handbook (3rd Edition). Stamford, CT: Cengage Learning
37. Durand, VM & Crimmins DB. (1992). The motivation assessment scale (MAS) administration guide. Topeka, KS: Monaco Associates.
38. Iwata BA & DeLeon IG. (1996). Functional analysis screening tool (FAST). Gainesville: Florida Center on Self-Injury, University of Florida.
39. Lewis TJ, Scott TM, Sugai G. The Problem Behavior Questionnaire: A Teacher-Based Instrument To Develop Functional Hypotheses of Problem Behavior in General Education Classrooms. Diagnostique. 1994;19(2-3):103-115. doi:10.1177/073724779401900207
40. Bijou SW, Peterson RF, Ault MH. A method to integrate descriptive and experimental field studies at the level of data and empirical concepts1. Journal of Applied Behavior Analysis. 1968;1(2):175-191. doi:10.1901/jaba.1968.1-175
41. Touchette PE, MacDonald RF, Langer SN. A scatter plot for identifying stimulus control of problem behavior. Journal of Applied Behavior Analysis. 1985;18(4):343-351. doi:10.1901/jaba.1985.18-343
42. Hanley GP, Iwata BA, McCord BE. Functional analysis of problem behavior: a review. Journal of Applied Behavior Analysis. 2003;36(2):147-185. doi:10.1901/jaba.2003.36-147
43. Iwata BA, Dozier CL. Clinical Application of Functional Analysis Methodology. Behavior Analysis in Practice. 2008;1(1):3-9. doi:10.1007/bf03391714
44. Hieneman M & Dunlap G. (2015). Implementing multi-element positive behavior support plans. In F. Brown, J. Anderson, & R. De Pry (Eds.), Individual positive behavior supports: A standards-based guide to practices in schools and community-based settings (pp.417-431). Baltimore, MD: Paul H. Brookes Publishing.
45. Todd AW, Algozzine B, Horner RH, & Algozzine K. (2014). Data-based decision making. In C. Reynolds, K. Vannest, & E. Fletcher-Janzen (Eds.), Encyclopedia of special education: A reference for the education of children, adolescents, and adults with disabilities and other exceptional individuals (4th ed.). Hoboken, NJ: John Wiley & Sons.
46. Sanetti LMH, Dobey LM, Gritter KL. Treatment Integrity of Interventions With Children in the Journal of Positive Behavior Interventions From 1999 to 2009. Journal of Positive Behavior Interventions. 2011;14(1):29-46. doi:10.1177/1098300711405853
47. Freeman R, Enyart M, Schmitz K, Kimbrough P, Matthews P, & Newcomer L. (2014). Integrating best practice in person-centered planning, wraparound, and positive behavior support to enhance quality of life. In F. Brown, J. Anderson, & R. De Pry (Eds.), Individual positive behavior supports: A standards-based guide to practices in school and community-based settings (pp 241-257). Baltimore, MD: Brookes Publishing.
48. Kincaid D, Knoster T, Harrower JK, Shannon P, Bustamante S. Measuring the Impact of Positive Behavior Support. Journal of Positive Behavior Interventions. 2002;4(2):109-117. doi:10.1177/109830070200400206
49. Luiselli JK. Antecedent Assessment & Intervention: Supporting Children & Adults with Developmental Disabilities in Community Settings. Paul H. Brookes Pub; 2006.
50. Richman DM, Barnard-Brak L, Grubb L, Bosch A, Abby L. Meta-analysis of noncontingent reinforcement effects on problem behavior. Journal of Applied Behavior Analysis. 2015;48(1):131-152. doi:10.1002/jaba.189 1.
51. Shogren KA, Faggella-Luby MN, Sung Jik Bae, Wehmeyer ML. The Effect of Choice-Making as an Intervention for Problem Behavior. Journal of Positive Behavior Interventions. 2004;6(4):228-237. doi:10.1177/10983007040060040401
52. Koyama T, Wang H-T. Use of activity schedule to promote independent performance of individuals with autism and other intellectual disabilities: A review. Research in Developmental Disabilities. 2011;32(6):2235-2242. doi:10.1016/j.ridd.2011.05.003
53. Kern L, Choutka CM, Sokol NG. Assessment-Based Antecedent Interventions Used in Natural Settings to Reduce Challenging Behavior: An Analysis of the Literature. Education and Treatment of Children. 2002;25(1):113-130. http://www.jstor.org/stable/42900519
54. Wheeler JJ, Carter SL, Mayton MR, Chitiyo M. Preventing Challenging Behaviour through the Management of Instructional Antecedents. Developmental Disabilities Bulletin. 2006;34:1-14. https://eric.ed.gov/?id=EJ815703
55. Durand VM, Carr EG. Functional communication training to reduce challenging behavior: maintenance and application in new settings. Journal of Applied Behavior Analysis. 1991;24(2):251-264Ti community (pp. 81-98). Baltimore: Paul H. Brookes.
56. Tiger JH, Hanley GP, Bruzek J. Functional Communication Training: A Review and Practical Guide. Behavior Analysis in Practice. 2008;1(1):16-23. doi:10.1007/bf03391716
57. Baker BL, Brightman A. Steps to Independence: Teaching Everyday Skills to Children with Special Needs. Paul H. Brookes Pub. Co; 2004.
58. Athens ES, Vollmer TR. AN INVESTIGATION OF DIFFERENTIAL REINFORCEMENT OF ALTERNATIVE BEHAVIOR WITHOUT EXTINCTION. Thompson R, ed. Journal of Applied Behavior Analysis. 2010;43(4):569-589. doi:10.1901/jaba.2010.43-569
59. Ingram K, Lewis-Palmer T, Sugai G. Function-Based Intervention Planning. Journal of Positive Behavior Interventions. 2005;7(4):224-236. doi:10.1177/10983007050070040401
60. Janney DM, Umbreit J, Ferro JB, Liaupsin CJ, Lane KL. The Effect of the Extinction Procedure in Function-Based Intervention. Journal of Positive Behavior Interventions. 2012;15(2):113-123. doi:10.1177/1098300712441973
- Albin RW, Lucyshyn JM, Horner RH, Flannery KB. Contextual fit for behavioral support plans: A model of “goodness of fit” In: Koegel LK, Koegel RL, Dunlap G, editors. Positive behavioral support: Including people with difficult behavior in the community. Baltimore: Paul H. Brookes; 1996. pp. 81–98.
62. Hieneman M, Dunlap G. Factors Affecting the Outcomes of Community-Based Behavioral Support. Journal of Positive Behavior Interventions. 2000;2(3):161-178. doi:10.1177/109830070000200304
63. Moes DR, Frea WD. Contextualized behavioral support in early intervention for children with autism and their families.Journal of Autism and Developmental Disorders. 2002;32(6):519-533. doi:10.1023/a:1021298729297
64. Smith-Bird E, Turnbull AP. Linking Positive Behavior Support to Family Quality-of-Life Outcomes. Journal of Positive Behavior Interventions. 2005;7(3):174-180. doi:10.1177/10983007050070030601
65. Duda MA, Clarke S, Fox L, Dunlap G. Implementation of Positive Behavior Support With a Sibling Set in a Home Environment. Journal of Early Intervention. 2008;30(3):213-236. doi:10.1177/1053815108319124
66. Lucyshyn JM, Albin RW, Horner RH, Mann JC, Mann JA, Wadsworth G. Family Implementation of Positive Behavior Support for a Child With Autism. Journal of Positive Behavior Interventions. 2007;9(3):131-150. doi:10.1177/10983007070090030201
67. Vaughn BJ, Clarke S, Dunlap G. ASSESSMENT-BASED INTERVENTION FOR SEVERE BEHAVIOR PROBLEMS IN A NATURAL FAMILY CONTEXT. Journal of Applied Behavior Analysis. 1997;30(4):713-716. doi:10.1901/jaba.1997.30-713
68. Sanders MR. Triple P-Positive Parenting Program as a public health approach to strengthening parenting. Journal of Family Psychology. 2008;22(4):506-517. doi:10.1037/0893-3200.22.3.506
69. Dishion TJ, Stormshak EA. Intervening in Children’s Lives : An Ecological, Family-Centered Approach to Mental Health Care. American Psychological Association, (Imp; 2007).
70. Dunst CJ, Trivette CM, Hamby DW. Meta-analysis of family-centered helpgiving practices research. Mental retardation and developmental disabilities research reviews. 2007;13(4):370-378. doi:10.1002/mrdd.20176
71. Jonkman CS, Schuengel C, Lindeboom R, Oosterman M, Boer F, Lindauer RJ. The effectiveness of Multidimensional Treatment Foster Care for Preschoolers (MTFC-P) for young children with severe behavioral disturbances: study protocol for a randomized controlled trial. Trials. 2013;14(1):197. doi:10.1186/1745-6215-14-197
72. Leve LD, Fisher PA, Chamberlain P. Multidimensional Treatment Foster Care as a Preventive Intervention to Promote Resiliency Among Youth in the Child Welfare System. Journal of Personality. 2009;77(6):1869-1902. doi:10.1111/j.1467-6494.2009.00603.x
73. Nowak C, Heinrichs N. A Comprehensive Meta-Analysis of Triple P-Positive Parenting Program Using Hierarchical Linear Modeling: Effectiveness and Moderating Variables. Clinical Child and Family Psychology Review. 2008;11(3):114-144. doi:10.1007/s10567-008-0033-0
74. McEachern AD, Fosco GM, Dishion TJ, Shaw DS, Wilson MN, Gardner F. Collateral benefits of the family check-up in early childhood: Primary caregivers’ social support and relationship satisfaction. Journal of Family Psychology. 2013;27(2):271-281. doi:10.1037/a0031485
75. Clark HB, Clarke RT. Research on the wraparound process and individualized services for children with multi-system needs. Journal of Child and Family Studies. 1996;5(1):1-5. doi:10.1007/bf02234674
76. Tumbull AP & Turnbull HR. (1996). Group action planning as a strategy for providing comprehensive family support. In L. K. Koegel, R L Koegel, & G. Dunlap (Eds.), Positive behavioral support: Including people with difficult behavior in the community (pp. 99-114). Baltimore, MD: Paul H. Brookes Publishing.
77. Walker JS, Schutte KM. Practice and Process in Wraparound Teamwork. Journal of Emotional and Behavioral Disorders. 2004;12(3):182-192. doi:10.1177/10634266040120030501
78. Clark HB, Hieneman M. Comparing the Wraparound Process to Positive Behavioral Support. Journal of Positive Behavior Interventions. 1999;1(3):183-186. doi:10.1177/109830079900100307
79. Chamberlain P & Smith DK (2003). Antisocial behavior in children and adolescents: The Oregon multidimensional treatment foster care model. In A. E. Kazdin & J. R. Weisz (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 282-300). New York: Guilford Press.
80. McCart A, Lee J, Frey AJ, Wolf N., Choi JH., Haynes H. (2010). Response to intervention in early childhood centers: A multitiered approach to promoting family engagement. Early Childhood Services, 4(2), 87-104.
81. Phaneuf L, McIntyre LL. EFFECTS OF INDIVIDUALIZED VIDEO FEEDBACK COMBINED WITH GROUP PARENT TRAINING ON INAPPROPRIATE MATERNAL BEHAVIOR. Journal of Applied Behavior Analysis. 2007;40(4):737-741. doi:10.1901/jaba.2007.737-741
82. Phaneuf L, McIntyre LL. The Application of a Three-Tier Model of Intervention to Parent Training. Journal of Positive Behavior Interventions. 2011;13(4):198-207. doi:10.1177/1098300711405337
83. Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology. 2000;68(4):624-640. doi:10.1037/0022-006x.68.4.624
84. Turner KMT, Sanders MR. Dissemination of evidence-based parenting and family support strategies: Learning from the Triple P—Positive Parenting Program system approach. Aggression and Violent Behavior. 2006;11(2):176-193. doi:10.1016/j.avb.2005.07.005
85. Webster-Stratton C. (2005). The incredible years: A training series for the prevention and treatment of conduct problems in young children. In: E. D. Hibbs, & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (pp. 507–555). Washington, DC: American Psychological Association.
86. Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology. 1997;65(1):93-109. doi:10.1037/0022-006x.65.1.93
87. Brinkmeyer MY & Eyberg SM. (2003). Parent-child interaction therapy for oppositional children. In A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 204-223). New York: The Guilford Press.
88. Fettig A, Barton EE. Parent Implementation of Function-Based Intervention to Reduce Children’s Challenging Behavior. Topics in Early Childhood Special Education. 2013;34(1):49-61. doi:10.1177/0271121413513037
89. Dunlap G, Newton JS, Fox L, Benito N, Vaughn B. Family Involvement in Functional Assessment and Positive Behavior Support. Focus on Autism and Other Developmental Disabilities. 2001;16(4):215-221. doi:10.1177/108835760101600403
90. Fettig A, Ostrosky MM. Collaborating with Parents in Reducing Children’s Challenging Behaviors: Linking Functional Assessment to Intervention. Child Development Research. 2011;2011:1-10. doi:10.1155/2011/835941
91. Wacker DP, Lee JF, Dalmau YCP, et al. CONDUCTING FUNCTIONAL ANALYSES OF PROBLEM BEHAVIOR VIA TELEHEALTH. Journal of Applied Behavior Analysis. 2013;46(1):31-46. doi:10.1002/jaba.29
92. Dunlap G, Ester T, Langhans S, Fox L. Functional Communication Training with Toddlers in Home Environments. Journal of Early Intervention. 2006;28(2):81-96. doi:10.1177/105381510602800201
93. Lucyshyn JM, Albin RW, Nixon CD. Embedding comprehensive behavioral support in family ecology: An experimental, single case analysis. Journal of Consulting and Clinical Psychology. 1997;65(2):241-251. doi:10.1037/0022-006x.65.2.241
94. Lucyshyn JM, Irvin LK, Blumberg ER, Laverty R, Horner RH, Sprague JR. Validating the Construct of Coercion in Family Routines: Expanding the Unit of Analysis in Behavioral Assessment with Families of Children with Developmental Disabilities. Research and practice for persons with severe disabilities: the journal of TASH. 2004;29(2):104-121. doi:10.2511/rpsd.29.2.104
95. Patterson GR. (1982). Coercive family process (Vol. 3). Eugene, OR: Castalia Publishing Company.
96. Eyberg SM, Funderburk BW, Hembree-Kigin TL, McNeil CB, Querido JG, Hood KK. Parent-Child Interaction Therapy with Behavior Problem Children: One and Two-Year Maintenance of Treatment Effects in the Family. Child & Family Behavior Therapy. 2001;23(4):1-20. doi:10.1300/j019v23n04_01
97. Herschell AD, Calzada EJ, Eyberg SM, McNeil CB. Parent-child interaction therapy: New directions in research. Cognitive and Behavioral Practice. 2002;9(1):9-16. doi:10.1016/s1077-7229(02)80034-7
98. Barton EE, Fettig A. Parent-Implemented Interventions for Young Children With Disabilities. Journal of Early Intervention. 2013;35(2):194-219. doi:10.1177/1053815113504625
99. Kazdin AE. (2005). Parent Management Training: Treatment for oppositional, aggressive, and antisocial behaviors in children and adolescents. New York: Oxford University Press.
100. Moes DR, Frea WD. Using Family Context to Inform Intervention Planning for the Treatment of a Child with Autism. Journal of Positive Behavior Interventions. 2000;2(1):40-46. doi:10.1177/109830070000200106
101. Koegel RL, Symon JB, Kern Koegel L. Parent Education for Families of Children with Autism Living in Geographically Distant Areas. Journal of Positive Behavior Interventions. 2002;4(2):88-103. doi:10.1177/109830070200400204
102. Dunlap G, Strain PS, Lee JK., Joseph J, Vatland C & Fox LK. (2017). Prevent-Teach- Reinforce for Families. Baltimore, MD: Brookes Publishing.
103. Bailey KM, Blair K-SC. Feasibility and potential efficacy of the family-centered Prevent-Teach-Reinforce model with families of children with developmental disorders. Research in Developmental Disabilities. 2015;47:218-233. doi:10.1016/j.ridd.2015.09.019
104. Sears KM, Blair K-SC, Iovannone R, Crosland K. Using the Prevent-Teach-Reinforce Model with Families of Young Children with ASD. Journal of Autism and Developmental Disorders. 2012;43(5):1005-1016. doi:10.1007/s10803-012-1646-1 1.
105. Bearss K, Johnson C, Smith T, et al. Effect of Parent Training vs Parent Education on Behavioral Problems in Children With Autism Spectrum Disorder. JAMA. 2015;313(15):1524. doi:10.1001/jama.2015.3150
106. Lucyshyn JM, Dunlap G, & Albin RW. (2002). Families and positive behavior support: Addressing problem behavior in family contexts. Baltimore, MD: Paul H. Brookes Publishing.
107. Hieneman M, Childs KE., & Sergay J. (2006). Parenting with positive behavior support: A practical guide to resolving your child’s difficult behavior. Baltimore, MD: Paul H. Brookes Publishing.
108. Durand VM & Hieneman M. (2008). Helping parents with challenging children: Positive family intervention: Facilitator guide/Parent workbook. New York, NY: Oxford University Press.
109. Durand VM. (2011). Optimistic parenting: Hope and help for you and your challenging child. Baltimore, MD: Brookes Publishing.
110. Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58(6-7):457-465. doi:10.1037/0003-066x.58.6-7.457
111. Elliott T, & Parker MW. (2012). Family caregivers and health care providers: Developing partnerships for a continuum of care and support. In R. C. Talley & J. E. Crews (Eds.), Multiple Dimensions of Caregiving and Disability (pp. 135-152). New York: Springer.
112. Madsen WC. (2007). Collaborative therapy with multi-stressed families. New York, NY: Guildford Press
113. Orchard CA, Curran V, Kabene S. Creating a Culture for Interdisciplinary Collaborative Professional Practice. Medical Education Online. 2005;10(1):4387. doi:10.3402/meo.v10i.4387
114. Whittingham K, Sofronoff K, Sheffield J, Sanders MR. Stepping Stones Triple P: An RCT of a Parenting Program with Parents of a Child Diagnosed with an Autism Spectrum Disorder. Journal of Abnormal Child Psychology. 2008;37(4):469-480. doi:10.1007/s10802-008-9285-x
115. Sanders MR, Bor W, Morawska A. Maintenance of Treatment Gains: A Comparison of Enhanced, Standard, and Self-directed Triple P-Positive Parenting Program. Journal of Abnormal Child Psychology. 2007;35(6):983-998. doi:10.1007/s10802-007-9148-x
116. Singh NN, Lancioni GE, Manikam R, Latham LL, & Jackman MM. (2014). Mindfulness-based positive behavior support in intellectual and developmental disabilities. In I. Iytzan & T. Lomas (Eds.), Mindfulness in positive psychology: The science of meditation and wellbeing (pp. 212-226). East Sussex: Taylor & Francis.
117. Hayes SC, Strosahl K, & Wilson KG. (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press.
118. Sanders MR, McFarland M. Treatment of depressed mothers with disruptive children: A controlled evaluation of cognitive behavioral family intervention. Behavior Therapy. 2000;31(1):89-112. doi:10.1016/s0005-7894(00)80006-4 1.
119. Allen KD, Warzak WJ. The problem of parental nonadherence in clinical behavior analysis: effective treatment is not enough. Journal of Applied Behavior Analysis. 2000;33(3):373-391. doi:10.1901/jaba.2000.33-373.
Permission to be Reprinted:
Journal of Child and Family Studies. October 2017, 25(2): 1-14.
DOI: 10.1007/s10826-017-0813-6
Keilman & Mishler | 70-81

Volume 10 ► Issue 4 ► February 2022
The Power of Collaboration through Behavioral Assessment and Treatment
Stacey Keilman, LCSW, and Lindy Mishler, MS
Abstract
Torrance State Hospital
(TSH) provides in-patient services for individuals with severe and persistent
mental health needs. This article presents the admission, assessment, and
treatment of a 55-year-old Caucasian man, referred to as DS with Intellectual
Disability, Schizophrenia, Chronic Paranoid Type, and Depression Not Otherwise
Specified (NOS). The initial assessment indicated significant trauma symptoms
in combination with undetected medical issues. However, treatments delivered at
TSH did not result in a clinically significant reduction in problem behavior. A
Functional Behavioral Assessment (FBA) was then completed to understand the
significance of DS's behaviors and provide strategies and supports that would
be beneficial to reduce the impacts of these actions, primarily in the hospital
setting. Direct and indirect data determined that the strategies resulted in a
significant decrease in behaviors while at TSH. Similar improvements occurred
in relationships with other patients and staff.
This article discusses the collaboration between State entities and the clinical implications of the assessments conducted.
Case Presentation
DS is a 55-year-old,
single, Caucasian male with a long history of admissions to community and State
hospitals. He was initially admitted to Torrance State Hospital due to
assaulting a nurse in a medical facility where he was seeking treatment for an
unknown medical issue. Upon admission, DS exhibited perseveration on thoughts
which included staff was going to cut off his testicles or people were
attempting to steal his items and keep them from him. He also showcased
significant anxiety due to not seeing his sister, with whom he previously had a
close relationship. He was then transferred to TSH's psychiatric unit due to
suicidal threats, self-injurious behaviors, and a significant regression in
self-care skills. Once on the psychiatric ward, staff described his behavior as
impulsive and physically aggressive towards other patients, staff, and
property. This included kicking, shoving, or charging at other patients; and
hitting, biting, or spitting at staff. He had also thrown food and drinks;
thrown or flipped tables; punched the walls; and often fell asleep laying on
the floor, preventing others from passing. DS also displayed self-injurious
behaviors such as hitting his head against something, scratching himself, and
throwing himself into a wall. In addition, staff observed DS becoming more
agitated after visits or phone calls with his sister. He would showcase refusal
behaviors with staff requests for taking medications or other task requests
during these times. During the initial presentation and throughout his hospital
stay, DS did not make staff aware if he was experiencing any pain, as evidenced
by his lack of expression when he experienced bleeding and lesions from extreme
jock itch, significant dental issues, and a corneal abrasion he received as a
result of a fight with another patient. Past medical issues included urinary
retention and acute renal failure, benign prostatic hyperplasia, GERD,
hypertension, kidney stones, hypercholesterolemia, and Chronic Obstructive
Pulmonary Disease (COPD).
Evaluation, Treatment, and Silos
Upon reviewing the referral information and prior records; it was identified that DS had a full-scale Intelligence Quotient (IQ) score of 56 from testing administered in early adulthood. This prompted consideration into potential involvement with other systems of care, triggering a conversation with DS's county mental health agency to identify historical information. This review identified that DS was involved with various community resources in the 1980s but was virtually unknown to the mental health/intellectual disability systems until 2006. Further, there was no agency involvement from 2006 to 2016. The mystery of how he maintained in the community for decades without involvement from the various human services systems required additional information since this could help develop strategies, supports, and resources to aid his discharge to community living.
Trauma
Shortly after hospital admission, a Torrance clinician conducted a comprehensive biopsychosocial assessment utilizing DS's sister as the primary source of information. The information gathered during this process uncovered medical issues and a significant change in his support system. Since his previous discharge in 2007, he lived with a caregiver for several years. During this time, he suffered some medical issues, including kidney stones. The arrangement with the caregiver ended, leading him to his psychiatric decompensation and hospitalization. This incident and the tragic loss of his mother in 2006 became two significant traumas affecting his stability.
Treatment
As a result of DS's self-injurious behaviors, he had been placed in several physical holds (a method of restraint with the outcome of purposely limiting physical movement), and a one-piece jumpsuit was ordered to be worn for his protection. His mood vacillated from withdrawn to irritable. At times, he was verbally and physically aggressive. He would become fixated on things and place himself on the floor when matters did not go as expected. He displayed the same perseverations as previously exhibited, and that he was going to die. He injured himself on three occasions by gouging at his wrists with a colored pencil, burning himself with a lighter, and attempting to cut off his genitals. He was an elopement risk during this time as well. The TSH Treatment Team had attempted various interventions to assist DS in gaining and maintaining safe behaviors, but he was not making significant improvements. The staff were demoralized over the lack of progress he was making, and DS expressed feelings of hopelessness. It soon became clear that the psychiatric interventions and strategies that TSH and staff had historically put in place were not effective on DS. Moreover, there was a need to consider other options.
Merging the Silos
When examining the health needs of people in Pennsylvania, the State health system tends to categorize by the individual’s cognitive and psychological, medical, and physiological needs. These divided mental, physical, and behavioral health sectors often complicate thorough treatments as a result of each operating independently from one another. Furthermore, there is no system in place where they can adequately share information across territories. Although this is not a new issue, its complexities have increased over time, causing holes where treatments are concerned. To begin the initial steps in merging the silos, the Office of Developmental Programs started the Capacity Building Institute (CBI). Torrance State Hospital (TSH) staff were invited to join a select group of professionals to meet with the intended goal of sharing philosophies and treatments while ultimately braiding together the mental, physical, and behavioral health territories. During these meetings, case presentations became a joint exercise for staff to share their entities' experiences and successes. It also provided a forum where other groups could recommend treatments or strategies that may not have been previously considered to improve the patient's treatment and address system issues. DS was one of the cases TSH chose to share due to his medical, psychological, and behavioral complexities.
One of the presentations by the Bureau of Supports for Autism and Special Populations (BSASP) was about the process and benefits of Functional Behavioral Assessment (FBA). It was explained that FBA is an evidence-based practice comprised of data collection to understand and recognize the purpose of specific behaviors exhibited by an individual. Once identified, the treatment team can decrease triggers and develop tailored interventions to eliminate problematic behaviors. In addition, the FBA is versatile because it can be used with anyone, in any setting, for any behavior.
Although TSH did have staff trained in the process of FBA, the general practice was not completed routinely, since this approach differs from the typical psychiatric treatment that has long been in place at TSH. Although treatments in State hospitals can be successful1, their interventions historically focused on mental health treatments2 rather than routine use of behavioral interventions to identify and decrease problematic behaviors. Since mental health treatments for the acute population have a significant focus on behavioral reduction rather than teaching new skills, interventions tend to be reactive rather than proactive, leaving the hospital staff in a cycle of crisis rather than proactive mitigation. To help address this issue, TSH requested BSASP complete an FBA on DS. Simultaneously, they also encouraged their staff to be trained in the FBA process, challenging the historical belief of enacting the otherwise unconventional therapeutic strategy in the state hospital setting and breaking down potential cross-system barriers.
Functional Behavioral Assessment3
Two clinicians from BSASP were assigned to complete the FBA at TSH for DS. The first step was to gather information about DS's behaviors. This indirect and direct information was collected through rating scales, assessments, direct observation of DS, interviews with hospital staff and DS's relatives, archived incidents, as well as record reviews. TSH freely provided access to the necessary people and resources for the BSASP staff to obtain the necessary information to be as comprehensive and holistic as possible. Using the information gathered on observed target behaviors, BSASP clinicians designed a customized data sheet for staff to collect additional information. This included the behaviors identified with the most significant and what occurred before and after the behavior. For accurate data collection and consistency across staff, it is considered good practice to ensure that the staff collecting the data have a thorough understanding of the expectations for recording the information. To assist with this, all staff were trained in using the datasheet prior to doing so. However, during the clinicians' initial analysis of the raw data, it was identified that there were still variances in the data being collected. As a result, both BSASP and TSH staff met to discuss confusion and revised the data sheets to make sense to the hospital staff to ensure accurate data collection. These revisions were proven successful after the next data set was analyzed, as evidenced by consistencies across staff in the raw data reviewed.
After collecting enough data to accurately represent all variables, BSASP staff graphed and analyzed the data to create a visual story of what the staff had been seeing over the course of the data collection period. Once developed, the graphs were compiled into a report. Without presenting their own hypothesis, BSASP presented the report to TSH staff and prompted conversation while encouraging staff to develop their own hypotheses based on what they were seeing in the data. Ultimately, TSH staff were able to use the visual analysis to develop their own story of what was occurring with DS, aligning with what BSASP hypothesized before meeting with the team. These similar observations were the foundation necessary to develop individualized recommendations.
Strategy recommendations are supports, strategies, interventions, and treatment recommendations grounded in information gathered and analyzed through the FBA process. They are completely reliant on accurate data, thorough data analysis, and hypotheses developed. Due to the quality put forth in the aforementioned steps, BSASP staff were able to identify the contributing conditions to DS’s problematic behaviors, how they can be addressed, any skills that needed to be taught, communication and social skill barriers, and how the environment and people were responding to DS’s behaviors. This resulted in developing operational definitions of the target behaviors, hypotheses of the functions of those behaviors, behavioral outcomes, and ideas for antecedent (before the behavior), replacement (during the behavior), and consequence (after the behavior has been completed) strategies. Although the strategy recommendations were linked to the hypotheses formulated from the indirect and direct data collected, they were also developed based on the ability of staff to complete them. Thus, a collaboration between BSASP clinicians and TSH staff was essential in developing and solidifying the final recommendation section. These comprehensive recommendations were later revisited to ensure they were effective and produced the intended results.
In order to shift the
staff’s responses from reacting to a crisis to being proactive and mitigating
risks, a Crisis Intervention Plan (CIP) was also developed. Using the
information gathered through the FBA process, BSASP staff were able to
recognize the situations that could be triggers for DS and precursor behaviors.
As a result, a CIP was developed that included triggers to a crisis, details to
assist in delineating the settings in which DS would be in and identify
de-escalation techniques for the TSH staff to implement.
The FBA process not only is designed to develop a list of strategy recommendations and CIP, but it can also be a means for identifying information otherwise undiscovered through its in-depth data collection and assessments. During the completion of DS’s FBA, interviews with DS and his sister identified that he had experienced more severe trauma than previously known. Some traumatic events included the deaths of multiple loved ones, including both of his parents and two close friends. He also experienced severe physical abuse from his previous girlfriend's children. Therefore, a Trauma-Informed Care (TIC) approach was critical to helping DS recover. Without the FBA, the central information regarding trauma would have continued to be missed and not addressed.
Conclusion
Following the FBA, TSH’s
treatment team began to see DS’s progress in maintaining safety. His mood
significantly improved, and he did not present any self- injurious behaviors
over time. In addition, his sister was actively involved in his treatment planning,
including providing historical information that assisted in medication
adjustments. Over the last few months at TSH, DS had gone on day passes with
his sister which had gone well and demonstrated that he was ready for
discharge. DS was ultimately discharged to a group with supports in place to
assist him in maintaining stability in the community.
It was not only DS that had benefited from the CBI’s collaboration. TSH staff experienced benefits as well. Through the FBA process, a data-driven, detailed, and thorough set of recommendations and strategies was made available to support the direct care staff. Torrance leadership supported staff to work with DS, setting a standard for staff to work towards and providing emotional support in times of stress and pressure. CBI became a champion for TSH and partners to come together, without the previous barriers and silos, to identify what DS needed to regain stability and return to his life in the community. The outcome for DS was a great success and demonstrated a complex culture evolution within the State hospital environment from the long-standing pure psychiatric treatment to eventually, total immersion with a data-based behavioral approach. Not only does this experience show the evolution and treatment progress of TSH, it also reflects the importance of collaboration from various stakeholders to meet individuals' complex and unique needs to ensure their long-term success.
References
1. Grossi PhD L, Osborn PhD L, Joplin MME, MT-BC K, O’Conner MS B. Clinical Interventions in State Psychiatric Hospitals: Safety and Logistical Considerations. Journal of Forensic Psychology Research and Practice. 2020;21(2):152-170. doi.org/10.1080/24732850.2020.1843105
2.
Geller
JL, Shore H, Grudzinskas AJ, Appelbaum PS. Against the Grain? A Reasoned
Argument for Not Closing a State Hospital. Psychiatric Quarterly.
2005;76(2):177-194. doi:10.1007/s11089-005-2338-y
3. Office of Developmental Programs. Functional Behavior Assessment Training. MyODP. https://www.myodp.org/course/view.php?id=1644
Biographies:
Stacey K. Keilman, LCSW: Stacey has been working in
the field of human services for 17 years. Her experience has
been focused in the areas of substance abuse and mental health treatment.
Her various roles have included assessment, treatment
planning and intervention, crisis de-escalation, case
management, social work administration, community discharge
planning, forensic administration, and hospital
administration. Stacey has held several leadership positions at Torrance
State Hospital including Social Work Supervisor, Social Work Manager, Forensic
Unit Director and is currently the Chief Executive Officer (CEO). Stacey
is a strong advocate for the individuals served at Torrance State
Hospital and embraces the Recovery Model.
Lindy Mishler, MS began working as a Clinical Consultant for the Bureau of Supports for Autism and Special Populations, Office of Developmental Programs in 2014. Lindy started her career as a Therapeutic Staff Support (TSS), where she discovered her passion working with children with autism. Since then, she has worked in a variety of positions, including direct support professional, vocational development, and has overseen Pennsylvania’s waiver programs in multiple agencies. Through these experiences, she has been able to expand her knowledge and experiences into other populations including adults with autism, traumatic brain injuries, other physical disabilities, and Mental Health diagnoses. She has a master’s degree in Psychology with a concentration in Applied Behavioral Analysis.
Contact Information
Stacey Keilman
Torrance State Hospital
Chief Executive Officer, LCSW
724-459-4511
Lindy Mishler, MS
Office of Developmental Programs, Bureau of Supports for Autism and Special Populations
Senior
Clinical Consultant
Nonnemacher | 82-90

Volume 10 ► Issue 4 ► February 2022
Putting the Positive in Behavioral Support: Considering the Role of Autonomy, Mastery, and Purpose
Stacy L. Nonnemacher,
Ph.D.
Introduction
We have made many strides in the understanding of effective behavioral support. Gone are the days of aversive strategies and interventions in the name of behavioral modification. We welcome the marriage of respectful, person-centered supports and science leading to long-lasting, meaningful changes in a person’s life.
Let’s Get on the Same Page
Everything we do is behavior. You are reading this article right now, that is a behavior. You may have used your mouse to scroll or picked up your coffee to take a sip while reading this article. These are all behaviors. At some point, we humans gave the word “behavior” a bad name. We all have behavioral repertoires, some work and some don’t support how we define living a meaningful life. And when someone we support is engaging in behaviors that may be interfering with their ideal functioning, we often say that the behavior is problematic and challenging. These descriptors are accurate but what we need to reconceptualize is who finds these behaviors problematic or challenging. Oftentimes, what the person is doing may be working for that person, while also being dangerous or disruptive. It may be their best attempt at getting what they want because they have no other functional way to communicate or may have historically been getting what they need as a result of engaging in this behavior. In a sense, this is working for them. However, the supporters of the person may find the behavior is not working; they are doing their best to provide support so that the person does not have to self-harm, hurt others, engage in property destruction, etc. to get what they need. In the end, the behavior is problematic or challenging to the people who support the person rather than to the person engaging in it to get their desires met.
Evolution
While much can be said about the evolution of behavioral support, for the purpose of this article, it is important to note that as the disability field has shifted from institutional to home and community support, we have worked to find better ways to support people across the lifespan. Behavioral science has moved from its early roots in theory to a focus on actionable consequences or finding ways to minimize behaviors, towards embracing a more person-centered, proactive approach that emphasizes the importance of quality of life and skill-building. Like any science, we continue to change and adapt based on what we learn as we practice and use technology to increase the precision of our implementation and research. Therefore, we land in a place where Positive Behavioral Support (PBS) marries the science from years of applied research and the art of individualized, person-centered supports.
Positive Behavioral Support
Positive Behavior Support is an approach to supporting people in home, school, work, and community environments that combines the principles of applied behavior analysis, implementation science, and best practices from other human service fields. It is characterized by a commitment to collaboration; basing interventions on a thorough understanding of the person and environmental influences affecting behavior; proactive, educative, and functional strategies; making decisions on the basis of objective information; and focusing not just on behavior change, but also on improvements in quality of life.1
PBS is predicated on several core features including1:
1. Data-Based Decision Making: PBS relies on objective data for decision-making. During assessment and through ongoing behavioral support, data is critical to guiding the direction of support.
2. Collaborative Team Process: PBS requires the engagement of individuals who are the focus of intervention and all relevant stakeholders. A multidisciplinary team is important to ensuring a holistic approach to assessment and intervention.
3. Assessment of Contexts and Functions: PBS requires objective and thorough assessments to develop effective, individualized support plans. Collecting both indirect and direct data to highlight patterns in function and contexts while also capturing broader physical and social ecology that might be contributing to the behavior is at the heart of PBS.
4. Multicomponent Plans: PBS plans include multiple components that are linked directly to the patterns identified in the assessment. Plans should include:
a. Preventative strategies.
b. Methods to teach replacement behaviors and other skills.
c. Interventions that focus on reinforcing positive behavior rather than problem behavior.
5. Lifestyle & Quality of Life Change: PBS is driven by the goal of improving people's quality of life. Finding purpose and meaning while focusing on improving advocacy, relationships, community engagement, productivity, and health and safety sets the stage for behavioral supports to work.
A Focus on Lifestyle and Quality of Life
“It is motivating when meaning and purpose are given to treatment beyond just avoiding offending behavior.” James Haaven2
While James Haaven speaks of treatment for persons who have sexually offended in this quote, it is a poignant consideration for all supporters. Avoiding the behavior of concern and focusing only on fundamental, physiological needs like food, shelter, and water ignores the importance of meaning and purpose as motivating qualities for someone to show up and have the drive to change – whether that is intrinsically or extrinsically motivated.
In fact, some assert that people who have their psychological needs to be competent, autonomous, and related to others met are also more motivated to grow and change – known as Self-Determination Theory3. This theory posits that physical and social environments that focus on meeting these psychological needs strengthen intrinsic motivation. Of course, there are times when extrinsic factors like rewards and praise are needed, but in a behavioral approach to treatment, we can do better in creating environments that focus more on getting these psychological needs met as a critical function in behavior change.
Dan Pink4 translated the Self-Determination Theory and other similar theories and research into a recipe of three easily understood ingredients that focus less on extrinsic desires and more on creating opportunities to foster autonomy, mastery, and purpose. We need to get better at embracing these three notions as central components of behavioral support.
Including Autonomy, Mastery, & Purpose in Behavioral Support
“Control leads to compliance; autonomy leads to engagement.” Daniel Pink4
- First, ask yourself how much autonomy someone has in their day. Taking inventory and seeing where someone is “decision deficient” could be very telling to how they are showing up and perhaps asserting themselves to seek control in a life over which they may feel they have no control.
- Second, mastery or being good at
something or just having the skills to accomplish a task motivates one to show
up time and time again even on the days you don’t feel like doing that task. If
you focus on ensuring that people have the skills they need to be successful,
they will engage and make progress.
Third, having a purpose, contributing to a larger goal, connecting with others, or sharing a common goal that is outside of ourselves bolsters the motivation of those who are autonomous and who have the skills to be successful. Finding meaning and purpose or something that a person is passionate about can make those other things bearable and more tolerable.
Conclusion
So, let us eliminate goals that focus on avoidance, and support plans that seek only to decrease challenging behavior. Instead, let us work on creating a system of support that seeks to provide opportunities for autonomous living where the person has the skills to be successful and finds or has purpose and connection outside of themselves. If we ground our behavioral support plans in the understanding that there is more than just minimizing, decreasing, or disruptive behavior; we can increase the chances that overall well-being and psychological health will be impacted. Consider James who was supported in the community with many restrictions to minimize his use of technology and social media due to a court order. James was described by his team as “unmotivated” and “resistant” to treatment. In fact, most of James’s day was spent playing video games and arguing with his staff about what he should be doing instead. James had a well-written Behavioral Support Plan (BSP) and while the team was able to put good antecedent and consequence strategies in place, they struggled to engage James in building skills like Activities of Daily Living (ADLs) and to follow through with things like scheduling his day. It wasn’t until a new, weekend staff person was hired that this began to change. The new staff person was the same age as James and talked with him as a peer. They talked about new things they could do together on weekends like go to clubs and bars. Long story short, the new staff person didn’t focus solely on correcting, controlling, and redirecting James. He gave James options to try new, age-appropriate things to occupy his free time (and he had a lot of it!) In turn, James paid more attention to his hygiene which prior to this, was one of the points of contention between James and his staff. We know that never ends well because, as in this case, the behaviors that were being addressed are looked at as “quality control.5” Unfortunately, this new staff person left his position as so many direct supporters do, and the focus on meaning and purpose was never written into James’s BSP, skills were not generalized, and the team returned to focusing on avoidance and decreasing challenging behavior. Thus, the team did not capitalize on the momentum of real behavioral change driven by a focus on autonomy, mastery, and purpose. We all know where that left James. Let this be a lesson to us all. Taking a behavioral approach in the treatment of challenging or interfering behaviors should consider both the art and science of support and an understanding and utilization of the PBS model to meet the needs of people like James and of those around him. Considering factors like autonomy, mastery, and purpose like James’s staff unknowingly did will provide the basis for engaging someone when teams feel all hope is lost. Acknowledging these positive changes and what is most influential in that change is important – even more important is to take what you learn and continue incorporating that in the supports for that person.
References
1. What is Positive Behavior Support? Home and Community Positive Behavior Support Network (HCPBS). https://hcpbs.org/what-is-positive-behavior-support/
2. Blasingame GD, Haaven J. Practical Treatment Strategies for Persons with Intellectual Disabilities: Working with Forensic Clients with Severe and Sexual Behavior Problems. Wood “N” Barnes Pub; 2006.
3. Deci E, Ryan R. Motivation, personality, and development within embedded social contexts: An overview of self-determination theory. The Oxford Handbook of Human Motivation. 2012.
4. Pink DH. DRIVE: The Surprising Truth about What Motivates Us. Canongate Books Ltd; 2018.
5. Hingsburger D. Power Tools: Thoughts about Power & Control in Service to People with Developmental Disabilities. Langara College; 2007.
Biography
Stacy L. Nonnemacher received her Ph.D. from Lehigh University. She is currently the Clinical Director for the Bureau of Supports for Autism and Special Populations in the Office of Developmental Programs in Pennsylvania's Department of Human Services. Stacy is the Editor in Chief of the Positive Approaches Journal. She has been involved in the field of disabilities for over twenty-five years supporting children, adolescents, and adults in home, community, and school settings. Dr. Nonnemacher has conducted applied research and training on Positive Behavioral Support, fostering self-determination, Functional Behavioral Assessment, and the needs of and support for individuals with autism.
Contact Information