Positive Approaches Journal, Volume 12, Issue 3
Malishchak | 45-53

Volume 12 ► Issue 3 ► November 2023
Alone: Suicide Prevention in the Pennsylvania Department of Corrections
Dr. Lucas D. Malishchak, DBA
Abstract
A recent cluster of suicides within the Pennsylvania Department of Corrections (PDOC) facilities led to a review of suicide data, identification of an inadvertent error in the data collection process, and numerous transformative revisions to PDOC’s suicide prevention efforts. Revisions have included but are not limited to single celling procedures, the utilization of suicide risk assessments with making housing decisions, and enhancements in understanding the connection between violence and suicide risk in prison, as well as the connection between State Correctional Institutions’ physical plant layouts and protective factors of suicide in prison.
A few years ago, the
Pennsylvania Department of Corrections (PDOC) experienced a cluster of suicides
within a short period of time. After each suicide, PDOC adhered to our standard
suicide clinical review process in an effort to identify areas of improvement
or needed remediation. Our Psychology Office also reviewed the cluster of
suicides together as a whole, to identify any broader systemic concerns that
may have occurred. In this cluster review, we identified that the percentage of
individuals categorized as “double celled” at the time of their death – meaning
they had a cellmate assigned to their cell – appeared high based on our
previous experience reviewing and understanding suicides. Consequently, we
re-reviewed each suicide within the cluster and discovered that in fact only
one of them was technically double celled at the time of the suicide; that is,
in only one instance was the cellmate present in the cell when the decedent was
discovered.
In the other four cases, although the individuals were categorized as double celled, they did not initiate the suicide until their cellmate was away or had exited the cell. The individuals were actually alone in the cell by themselves at the time they initiated their suicide. Upon discovering this inadvertent data collection error, we initiated a larger retrospective review of all suicides that had occurred within PDOC since 2000 in an effort to clarify the precise housing status of each decedent at the time of their discovery. Looked at through the lens of our new understanding of the concept of being double celled versus being alone, our review of this larger dataset revealed the same error in our understanding and categorization of housing status. The result was staggering: in 95% of all suicides that have occurred within the PDOC since 2000 – 174 of 184 – the individual was alone in a cell at the time of the suicide. The pie chart on the next page tells the entire story.
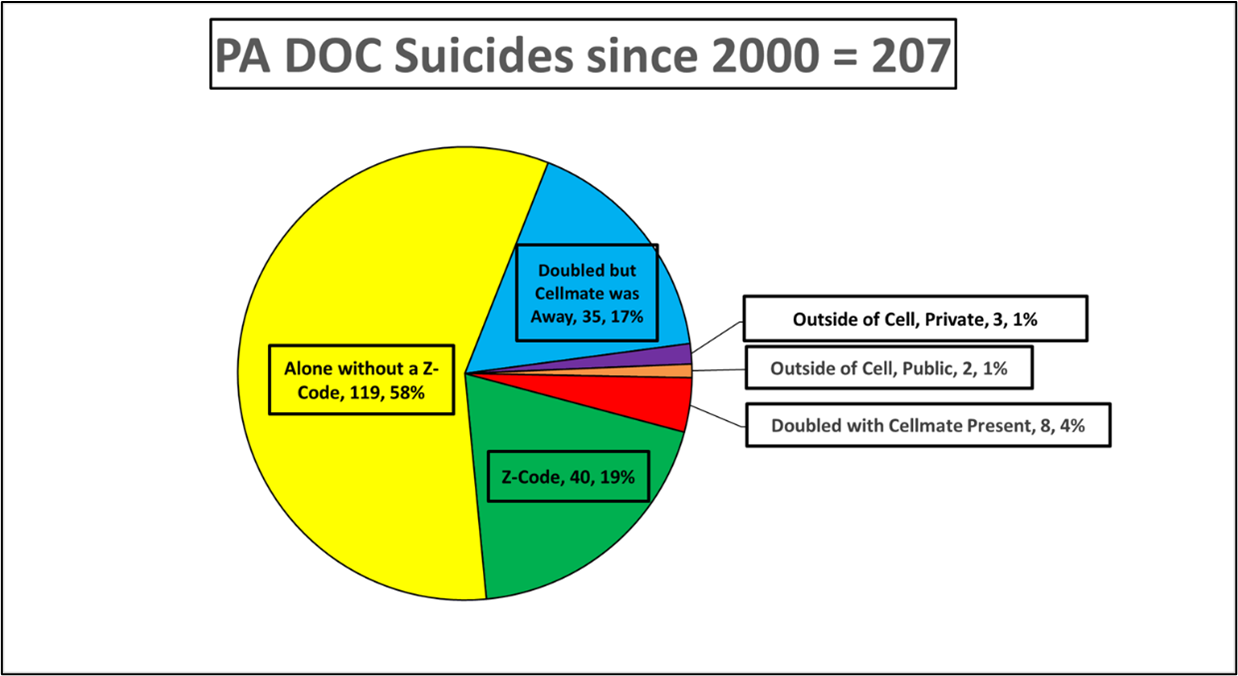
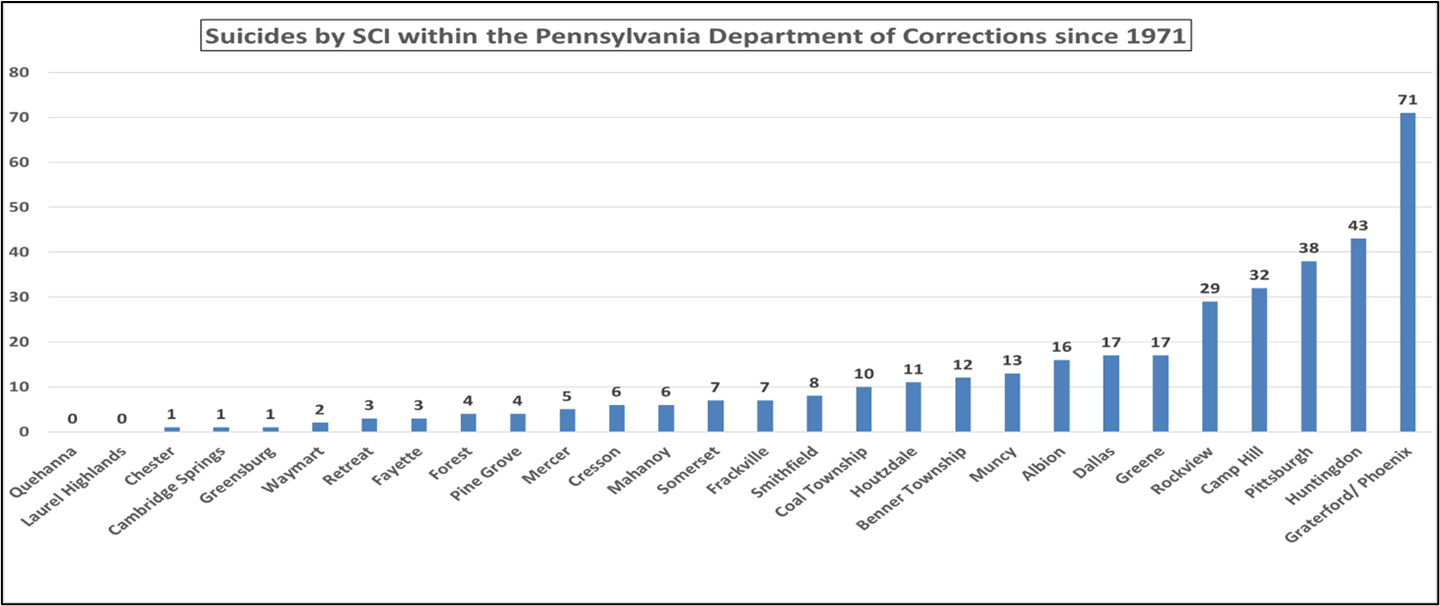
For reference, a Z-code indicates the person is assigned to a single cell (i.e., they are not assigned a cellmate). Once we discovered the “alone” issue, we wanted to further examine the data beyond our categorization error. We thought it would be helpful to know which specific PDOC prisons had experienced the most suicides during the past 50 years, so that we could strategically focus planned corrective interventions. We plotted exactly where – at which state correctional institution – each of 342 suicides had occurred since 1971.
Asking the Right Question
The 50 years of data revealed that certain prisons had experienced significantly more suicides than others. We asked ourselves, “What are those institutions doing so wrong?” It seemed obvious that we would find what we needed to know in the answer to that question. After some deliberation, we realized at least two reasons those prisons had experienced the most suicides: they have been open the longest, and they are some of our largest prisons. It immediately became clear that we were asking the wrong question. The better question was, “Which prisons have had the fewest suicides and why?” We identified four State Correctional Institutions (SCI) that were at least 30 years old and had very few suicides: Quehanna Boot Camp, SCI-Cambridge Springs, SCI-Laurel Highlands, and SCI-Waymart.
We were surprised to find that all four
facilities house populations known to be at increased risk of suicide: Quehanna
Bootcamp houses and treats predominantly younger (under 40) people with drug
and alcohol treatment needs. SCI-Cambridge Springs specializes in housing
females, who report or experience higher rates of mental illness and serious
mental illnesses than men. SCI-Laurel Highlands specializes in delivering the
highest level of acute medical care in our system, including care for people
who are terminally ill or near end of life. SCI-Waymart is responsible for delivering
PDOC’s highest level of inpatient mental health care and specializes in housing
our most seriously mentally ill male individuals. Despite high-suicide-risk
patient populations, those four SCIs, looked at together, had only ever
experienced two suicides. That finding was counterintuitive to what we thought
we knew about suicide risk. How were those institutions, which house apparently
higher-risk populations, having so much success at preventing suicides?
We informally interviewed staff from each
of the prisons and asked, “What are you doing differently?” Their answers were
consistent: "We’ve learned how to work effectively with these populations.
We know how to keep them safe. We treat them professionally and humanely; we
speak to them and treat them with respect." That seemed like a plausible
explanation, but it didn’t quite fit with what the data was telling us. While
we agreed that our staff at these institutions were professional, we thought
there may be something more going on, and in fact there was. At each of these
four prisons, there are very few cells. Most of their physical plants are
essentially open-dorm style settings. Most individuals are housed in large open
areas, visible to many other people, which creates infrequent “alone time.” In
addition to their excellent staff, one potential reason these prisons had so
much success in preventing suicides was that the individuals in these settings
were rarely housed alone.

Suicide
and the Pandemic
The number of suicides
recorded in PDOC prisons since the beginning of the COVID-19 pandemic appears
to corroborate the psychology office’s data findings. Given the significant
change, stress, loss, and unpredictability associated with this crisis, one would
expect the number of suicides to rise. During COVID, however, the total number
of suicides within PDOC prisons decreased by more than 50%, compared to the
same amount of time immediately preceding the start of the pandemic. How do we
explain that significant reduction? It might have been our reduced population,
a new Suicide Risk Assessment tool, enhanced training and communication, better levels of
supervision, or maybe even something else. One of the preventative actions
PDOC, like other correctional jurisdictions enacted to mitigate the risk of
spreading COVID-19, was to enhance movement restrictions within our population.
Many activities that during normal operations take people out of their cells
and create an opportunity for those who are double celled to be alone – for
instance going to school, work, or even to the day room to play chess – were
suspended. In an effort to protect our staff and population from spreading
COVID-19, we unintentionally decreased the amount of time alone experienced by
those who were double celled. We believe this partly explains why PDOC did not
have a single suicide categorized as “Doubled but cellmate was away” throughout
the entire pandemic, but had
experienced at least one of those types of suicides in 16 of the 18 years prior to the pandemic.
After putting all the
pieces together, it seemed clear to us that double celling or having a cellmate
present is a strong protective factor against suicide.
Our next step was to critically review our operational policies and practices. We began with a review of our Z-code policy, which outlined operational standards and guidelines for single and double celling. We discovered that our Z-code policy indicated that having mental health problems or a history of being dangerous toward self, self-mutilative, or unable to care for self were acceptable singular reasons to consider housing someone in a single cell. Our data, however, suggested that those reasons, taken alone, were likely contraindicated for being housed alone. As a result, we took immediate action and issued a memo to the organization revising the Z-code policy to prohibit assigning Z-codes for those contraindicated reasons. Additionally, we directed that all SCIs commence meaningful reviews of all individuals single celled at that
time to determine whether the individual could be safely double celled. Other improvements we have implemented, based on this suicide data review:
- Increased the frequency of security rounds on all Restrictive Housing Units and Special Management Housing Units statewide, from once every 30 minutes to unpredictable intervals with no more than 15 minutes between checks, with special emphasis on those individuals housed alone. By increasing the frequency of security rounds, we decreased the amount of time that people who are housed alone, are alone.
- Increased emphasis on out-of-cell clinical encounters with individuals housed alone on all Restrictive Housing Units and Special Management Housing Units, by assigning additional psychology staff to these units.
- Developed enhanced psychological evaluations for Z-codes, which now include a suicide risk assessment, violence risk assessment, review of objective testing, review of records, patient interview, and discussion with other staff members who know the patient well.
- Augmented pre-service and annual in-service suicide prevention trainings for all contact staff to include the results of this data review and relevant operational updates. Additionally, we emphasize that all other suicide prevention efforts currently in place must continue.
Through this process, the PDOC’s Psychology Office explored possible explanations for this “Alone Effect.” We tried to answer the question of why prison suicides appear to happen so rarely among people who are double celled but so often amongst those who are housed alone. The Psychology Office believes there are several potential explanations. First, if a cellmate is present, that cellmate can provide immediate rescue or intervention (i.e., to the person who is attempting suicide). Similarly, if a cellmate is present, that person can immediately call professional custody staff for help. Also, if a cellmate is present, that person may act as a deterrent simply by being present. A cellmate, if present, may offer protection against the fluctuating nature of suicide risk and or inaccurate assessments of suicide risk by correctional professionals. Likewise, if a cellmate is present, their presence may offer protection against those who falsely deny suicide intent to correctional professionals. Additionally, we believe that if a person is double celled with another person, their chances of developing their social support network, a known protective factor against suicide, is greatly increased. Finally, we believe there is a strong association between people assessed to be at high risk of violence and increased risk of suicide in prison, given that one of our primary violence risk mitigation interventions in prison is to cell violent people alone.
And that is how a fortuitous error helped advance PDOC’s understanding of suicide prevention and led to transformative changes.
Reprinted with permission from the National Commission on Correctional Health Care, CorrectCare magazine, copyright 2022.
Biography
Dr. Lucas D. Malishchak has been the Director of the Psychology Office for the Pennsylvania Department of Corrections since 2017. In this role, Lucas oversees a team of four Regional Licensed Psychologist Managers, who are together responsible for the clinical and administrative oversight of the mental health care system of Pennsylvania’s 24 State Correctional Institutions, which includes an infrastructure that supports more than 35,000 incarcerated people and more than 300 mental health care professionals. Lucas’ Doctor of Business Administration degree included a specialization in Criminal Justice. His dissertation was titled, “Alternatives to Segregation and Seriously Mentally Ill Inmates in Pennsylvania State Prisons: A Case Study of Employee Perceptions.”
Contact Information
Pennsylvania Department of Corrections
1920 Technology Parkway
Mechanicsburg, PA 17050
717-728-2093