Positive Approaches Journal, Volume 9, Issue 1
Gosselin & Sands | 27-54

Volume 9 ► Issue 1 ► 2020
Collaboration to Continuity: A Case Study Narrative on Berks County’s Mental Health
Forensic Diversion Program
Brandon Sands and Jillian Gosselin
Abstract
The number of individuals with mental illness diagnoses incarcerated each year continues to grow. Individuals with mental illness diagnoses often stay in jail longer, are less likely to post bail than those arrested for similar offenses and are more likely to experience significant delays in case processing than those who do not have a mental illness diagnosis1. “Research has identified that the criminal justice system may contain bias toward individuals with mental health diagnoses and has documented instances of improper treatment of individuals with mental health diagnoses while incarcerated2.” While many jails and prisons continue to be ill-equipped to provide adequate mental health care; these facilities are often where individuals first receive treatment and are identified as having a mental health condition2. Incarceration often exacerbates already present mental health symptoms and lends itself to the development of additional mental health concerns.
Introduction
Prevalence of mental illness diagnoses among local jail inmates are very high. One in six inmates who had a mental illness received treatment since detainment. Just over a quarter (26%) of jail inmates who had a diagnosed mental illness, compared to a fifth of those without, had served 3 or more prior incarcerations2. While incarcerated, 19% of jail inmates with mental illness were charged with violating facility rules compared of to only 9% of the overall inmate population. Those with a mental illness were three times as likely to be injured in a physical altercation since admission (9% compared to 3%).
The majority of offenses being committed by those with mental illness are minor such as trespassing, public intoxication, and other nuisance offenses3. These individuals are often arrested multiple times for similar offences over short periods of time and their risk for arrest is often increased due to substance use, homelessness, and unemployment.
Mental Health (MH) disorders are highly correlated with substance abuse (SA). About 76% of local jail inmates who had a mental health diagnosis also met criteria for substance dependence or abuse2. There are an estimated 4.2 million adults living with a Co-Occurring Disorder (CODs), which is a diagnosis of mental illness along with a substance abuse diagnosis4. Many times, CODs can influence and aggravate each other when left untreated2. Although improving considerably, only 12% of offenders with CODs received services for both disorders in 20122. Over 76% of State inmates with a MH disorder have a co-occurring SA disorder. Inmates with CODs have much higher rates of homelessness (133% higher), past physical or sexual abuse (58% higher) and parents who also were abused (71% higher)2.
Due to offenders facing multiple barriers to rehabilitation and crime-free lives and those with mental illness diagnoses being at a substantial disadvantage, forensic diversion and The Stepping Up Initiative were developed. Forensic diversion aims to assist an individual with mental illness to avoid or reduce jail time by linking them to community services. In many cases, where their charges are minor and the sanctions are limited, individual can be linked to community-based services without any reduction in jail time5. In diversion programs, early screening and engagement is key to minimizing contact with the justice system and even avoiding a short jail stay. The Stepping Up Initiative acknowledges that those with mental illness are overrepresented in the jails and are taking a toll on the criminal justice system.
Stepping up Initiative
The Stepping Up Initiative was launched in 2015 by the National Association of Counties, the Council of State Governments Justice Center, and the American Psychiatric Association Foundation to mobilize local, state, and national leaders to achieve a measurable reduction in the number of individuals in jail who have mental illness as the number of those incarcerated with mental health illness diagnoses has far surpassed those receiving treatment in hospitals. Berks County was chosen as one of eleven Innovator Counties across the nation and the first in Pennsylvania who are using the Stepping Up suggested three step approach which includes establishing a shared Serious Mental Illness (SMI) definition across criminal justice and behavioral health systems, ensuring everyone who is booked into jail is screened for a mental illness diagnosis, and regular reporting on this population.
Mental Health Forensic Diversion & Case Management Program in Berks County, Pennsylvania
Forensic Diversion is a program of the Berks County Mental Health & Developmental Disabilities Program (MH/DD) in partnership with Service Access Management Inc. (SAM) to reduce the incidences of individuals with identified and/or suspected mental illness from being incarcerated, reduce lengthy stays of incarcerations due to lack of supports, and decrease recidivism and/or police contact after release from higher levels of care. The Diversion team consists of the individual served, MH/DD, Diversion Specialist and Forensic Blended Case Manager, Criminal Justice Agencies (Police, District Attorney, Jail, Probation/Parole, and Public Defender), mental health agencies, and family members.
The Diversion Specialists (both licensed clinicians) meet with individuals to determine if they are appropriate candidates for services. Appropriateness for services is defined as a person living with the following: mental illness diagnosis, current criminal justice involvement, and reduced imminent risk to the community. If an individual is deemed appropriate for a diversion plan, the Diversion Specialist will make recommendations to the Courts as to specific conditions to reduce and/or eliminate charges. Some conditions may include; stipulated treatment compliance, compliance with medication management, participation is assigned community wellness programs, and oversight with mental health case management supports. Most commonly, these stipulations are regulated with unsecure bail conditions which are then monitored through Pretrial Services. Forensic Blended Case Managers (FBCM) monitor compliance to the Mental Health Forensic Diversion Program and meet weekly with individuals on an active diversion plan. If conditions are not followed and the person is not engaging in services, bail can be revoked, and further criminal charges pursued.
Within the past 2 years, the Mental Health Forensic Diversion Program (MHFDP) in Berks County expanded to include 17 one bedroom, fully furnished Forensic Housing apartments in partnership with another local treatment provider to address the issue of homelessness that many individuals face. Every individual who is accepted into the Forensic Housing program works with a housing case manager through a contracted agency as well as a FBCM through SAM.
The goal of FBCM is to assist individuals, both currently in the penal system and former inmates, to connect to the system of supports and programs available that help them achieve their wellness and recovery goals. FBCMs meet with individuals within the county jail system to determine eligibility for case management, assess individual’s needs, and develop goals prior to their release. Forensic case managers also assist released individuals to access appropriate community resources and coordinate mental health services.Sequential Intercept Model
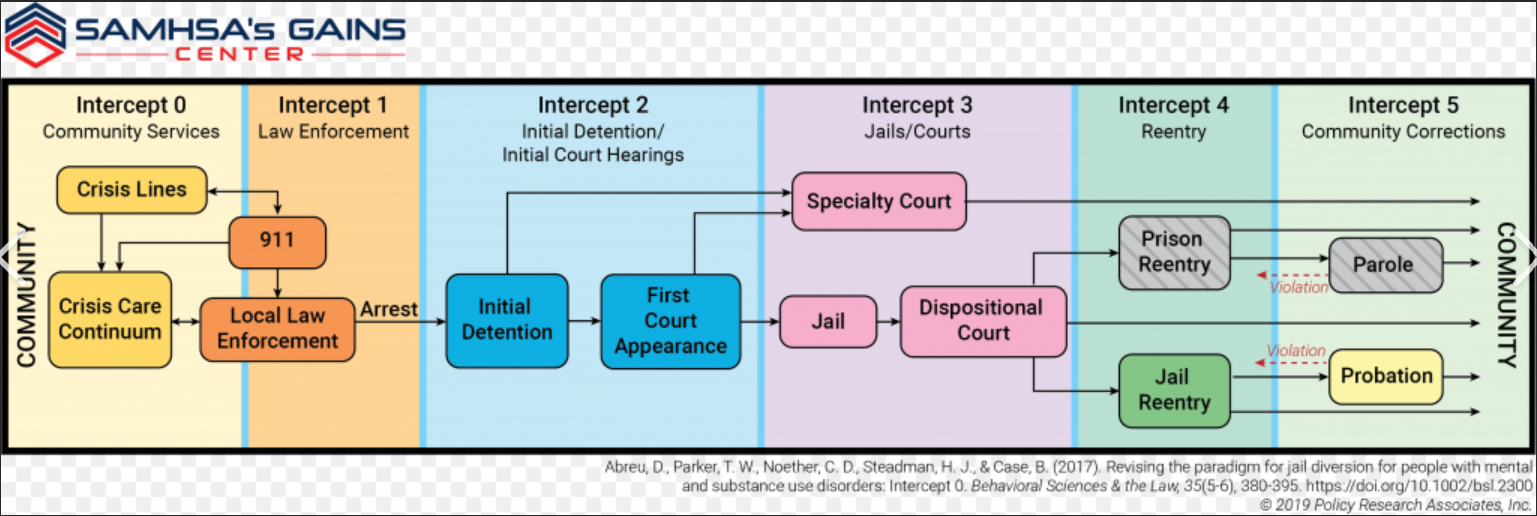
As stated above, individuals with mental illness are overrepresented in jails and prisons. It has been our program’s observation that correctional facilities are not intended to be mental health treatment facilities and are unable to service in this capacity. In addition to mental health symptoms worsening during incarceration, individuals experience a disruption in treatment as well, if they were receiving community-based treatment prior to their arrest and detainment. The Sequential Intercept Model (SIM) outlines several points at which a person with mental illness can be “intercepted” and kept from going further into the justice system (see Chart 1 below). Berks County’s Diversion Specialists utilize the SIM for every diversion. Six different intercepts have been identified by the SIM: Intercept 0: Community Services encompass the early intervention points for people with mental health issues before they are arrested and involves other agencies outside of the justice system such as Crisis Intervention services; Intercept 1: Law Enforcement and/or other first responders are often the first to encounter an individual experiencing a mental health crisis. This intercept includes all pre-arrest diversion options and concludes when someone is arrested; Intercept 2: Initial Detention/Initial Court Hearings include post arrest diversion options which include treatment instead of incarceration or prosecution. Strategies are used at this Intercept to screen for mental health issues, divert individuals through pre-trial services for low level offenses with treatment; Intercept 3: Jails/Courts concentrate on individuals who are being held in pretrial detention and are awaiting disposition of their criminal case(s). Specialty treatment courts may be offered at this intercept; Intercept 4: Reentry addresses continuity of care between the jail system and mental health providers in the community; and, Intercept 5: Community Corrections includes probation and parole and offers alternatives to technical violations that would usually result in jail time. Diversion specialists can engage an individual with mental illness at any one of these six intercepts.
Chart 1. Sequential Intercept Model
Berks County Mental Health Forensic Diversion Program Overview and Case Studies
The Berks County Mental Health Forensics Program was developed January of 2011. Its initial growth came from a collaborative joint effort between Berks County’s Office of Mental Health and Developmental Disabilities (MH/DD) and the county’s pre-trial service provider with a preliminary focus to offer diversionary assessments and evaluations for defendants at the Common Pleas Level of pretrial judiciary commitments. With an initial purpose to integrate diversionary supports and options that would serve as alternates to incarceration of the “mental health forensics” population, early findings concluded that a broader scope of what a mental health forensics population would need to be redefined.
As the program developed and more focus was on redefining the mental health forensic population, it became clear that more intercept and diversionary efforts were needed at the arresting intercept point. Berks County quickly began a course of mental health forensics training, education, collaboration, and communication with all judiciary, criminal, justice, law enforcement, and mental health stakeholders. Numerous levels of intercept mapping were developed to help assess where the largest need was present and to intercept non-imminent risk mental health arrests, provide jail diversion at the pre-arrest point, and decrease non-imminent risk defendants at the magisterial district court and arraignment intercept points. It is with these intercept points of recognition that the Mental Health Forensic Diversion Program (MHFDP) was created and implemented real time psycho-forensics assessments at the arresting intercept point.
Berks County’s MHFDP quickly became a resource for Berks County’s 42 different law enforcement departments. The police department’s reception of the MHFDP was nothing short of outstanding. By offering the police departments a specialized program that increased police officer awareness and training in dealing with mental health contacts, the number of incarcerated, low-risk mental health offenders decreased.
To date, 633 mental health forensics diversions over the past eight years have been completed including 326 police encounters interventions and only 33 cases of re-arrest by diversion clients while in the program. Finally, the most impactful and prideful fact, of the 326 arrest point diversions with police, only twice did a police officer disagree with the recommendations at two separate intercept points. This demonstrates the exceptional quality of collaboration, community support, and citizen empathy that occurs when varying county offices are in complete agreement with and understand the need to improve mental health supports.
Below are two case examples that will highlight our programs efforts in supporting the mental health forensics population.
Presentation of Mental Health Forensic Diversion Intercept Point Case Examples
Case Example I: John Doe Mental Health Forensic Diversion Intercept Point 3(A2)
Mental Health Forensic Intercept Narrative (A2) for John Doe
Berks County Mental Health Forensics Program received a contact from a rural police department in Berks County asking for a diversion specialist to complete a psycho-forensic evaluation for diversionary options on scene where several imminent risk factors are present: self-harm, threats of harm, weapons, and aggregated assaultive behavior. The Police Officer on scene also reported that, despite the imminent risk threat, he is concerned that John Doe may have underlying mental health concerns, and that jail may not be the most appropriate level of care for John Doe.
Mental Health Forensic Presenting Narrative (A2):
The psycho-forensic diversion specialist arrived on scene to a moderately secluded single home in a rural township of Berks County. On scene were five police officers, two EMT’s, and two firefighters. Along with the first responders are John Doe, his mother, father, brother, and four on-looking neighbors. The time of day was approximately 8:30pm on a Friday in late summer. The home was clean but unorganized.
The police officer reported that John Doe and his sibling engaged in a physical altercation, of which John Doe threatened to kill his brother with a knife. The police officer reported there have been multiple calls to the home for similar complaints and added that there is a history of marijuana and alcohol use in the home and by the brothers. It was also reported that John Doe had written $5,000.00 worth of fraudulent checks from his father’s checking account. John Doe used the checks to purchase a cache of firearms, parts, and accessories. The police reported no known criminal behaviors to harm others or threats of illicit weapons usage.
In meeting with John Doe’s mother and father, both report an exacerbated history of mental health treatment and medical concerns. They reported that John has been diagnosed with various mental health disorders over the past four years and that John Doe displays erratic and psychotic type behavior. The parents reported that John has active charges pending in another county for a DUI, trespassing, and damage in excess of $1,000.00. These charges were a result of John becoming agitated and aggressive after an altercation with his brother over a video game which led John to consume alcohol and smoke marijuana, which led to him crashing his car into a local grocery store. His mom reported that behavior as being out of character for him.
During conversation, his parents reported that they have been divorced for three years. They described their relationship as poor at best and the family’s typical home life is unhealthy and unsupportive. Dad reported that John’s grandfather is an avid gun collector who taught John about the craft of making firearms. Dad continued to report that John is a marksmen on several area shooting clubs and that John possesses the ability to hit a bullseye from 300 yards away, and that he was very concerned as John decompensates more frequently. It was explained that John was a straight A student as a high school sophomore three years ago. John suffered a concussion from football three years ago and that they noticed depressive fugue type states. Additionally, John experienced three more concussions since his sophomore year in high school and the concussions went primarily untreated; although, he did seek medical attention via area emergency departments.
Brief Real Time Psycho-Forensic Assessment (A2)
A real time psycho-forensic assessment was conducted on scene to determine the motive of criminal behaviors, psychopathology, and imminent risk. Upon meeting with John, it was evident that he was experiencing acute features of anxiety, instability of thought, and mild depressive features. His overall presentation was best described as engaging in posture, articulate of content, and distracted in reality-testing. He did not present any psychotic features or expressions of self-harm. He was easily distracted by the overall energy surrounding the current intervention. He reported acute and heightened anger feelings and thoughts as explained by John: “sometimes I get like this and I don’t know why, my brother really did nothing wrong. I just get so angry and I can’t control it.” He continued to state, “I don’t hear voices, I don’t usually feel out of control, I never want to hurt anyone. Just I get this feeling when I can’t think right. Like my brain is out of control.” John reported an extensive history of acute, unprovoked angry states. He described these states as out of his control and reckless. John reported some drug use with marijuana and minimal alcohol use, which began about 2 years prior.
As the conversation continued, John maintained a cooperative and engaging tone and posture. He appeared labile for the most part of our conversation, and was talkative and expressive; however, his mood was flat. He continued to state, “I probably would have killed my brother and I have no idea why. I just get so angry I don’t know why.” When asked about the cache of firearms parts he purchased with his father’s blank checks he replied, “I don’t know what I was going to do with them, probably nothing good.”
It is also noted that John’s family offered the following information: John had multiple concussions that were untreated the past four years, he had numerous mental health interventions and treatment with minimal success, John is highly intelligent and had full academic scholarships to three universities, and he has displayed unprovoked aggressive and dangerous behaviors multiple times since his first concussion.
The following recommendations were made as a result of the assessment and rationale: detainment to jail on the current charges was needed to eliminate any imminent risk and provide a level of safety for John and the community, of which he would not receive in an inpatient mental health facility. John presented with several Traumatic Brain Injury (TBI) markers that lead this writer to rule out mental health primary concerns; due to this, an inpatient psychiatric admission would serve no current purpose. Exploration of adequate treatment options for John’s underlying traumatic brain injury pathology would be determined while decreasing all imminent risk possibilities.
Based on forensic diversion recommendations and after consultation with the arresting police officers and the Berks County District Attorney’s office, John was detained at jail. Subsequent diversionary actions began to explore a level of adequate treatment for John related to TBI pathology and treatment.
Jail-Based Diversion Planning (A2):
John was placed in a single cell on the jail’s medical unit. During several meetings and assessments with various providers and professionals, John continued to display excellent compliance with all jail programming, willingness to learn about his mental and cognitive concerns, and an excellent level of investment into stabilizing his impulsive and unexplained anger outbursts. He stated, “I just feel that sometimes my brain loses track of what I’m doing and makes me so angry. Like I can be reading about history and all of a sudden, I want to hurt someone. I don’t hear voices, it’s like a switch just flips.”
John continued to report TBI type effects while in jail and during the time the diversion specialist met with him at the jail to build rapport. He stated, “My head just hurts sometimes, I get headaches all the time. I throw up without warning. Flickering lights cause so much pain in my head.” John started reporting these symptoms during the first meeting while he was in jail. It was evident that his TBI pathology was his primary health concern and that there are no mental health markers that should be considered at that point. From a pathology of behavior understanding, it became clear that John needed TBI and Cognitive Rehabilitation supports and not psychiatric intervention.
The forensic team started a course of research into TBI and Cognitive Restorative Programs in Pennsylvania which uncovered a new State funded program for “Early Onset TBI Rehabilitation.” This program is grant funded and awarding of the state grant requires several levels documentation that included historical and demographic information, current assessments, medical TBI evaluations, social relationships, and academic performance. The team quickly prepared the referral packet and began the referral process. After approximately two weeks, the referral packet for TBI state programming was accepted and the residential program director of TBI Rehabilitation agreed to meet John at the jail. The program director and her team conducted four separate assessments with John while he was in jail and it was determined that John was an ideal candidate for TBI Rehabilitation. They agreed to award him a grant of $200,000.00 for 16- month admission into their TBI Cognitive Rehabilitation Residential Program (CRRP). His official acceptance and move-in to the program would occur in about four months.
Once the team received confirmation of John’s acceptance into the CRRP, the district attorney and John’s legal defense were notified. It was recommended that John remain in jail for the next three months to continue his course of stabilization with jail-based reentry programming and that John be released one month prior to the CRRP admission and admitted into the Mental Health Forensic Diversion Housing Program (MHFHP). The goal for his admission into our MHFHP was to prepare John for re-integration into a program-based setting while under a supervised supportive structure.
The district attorney’s office, John’s legal defense, and the judge agreed with the recommendations of the forensic diversion specialist. An unsecured bail plan was filed, and John was ordered to comply with all diversion conditions of the bail plan.
Unsecured Bail Diversion Plan (A2)
John was released from jail approximately three months after his arrest for charges of aggravated and simple assault, harassment, possession and administration of fraudulent checks, possession of illicit firearms in excess of $5,000.00, and terroristic threats. He was placed on unsecured bail and the charges were to be held for continuance through his admission into Berks County’s Mental Health Forensic Program.
John’s unsecured bail conditions-based diversion recommendations were as follows:
For one month, or until admission into the CRRP, you will comply with all conditions of your bail:
1. Maintain compliance with all the rules and conditions of the MHFHP
2. Maintain compliance with all of you outpatient treatment requirements
3. Begin a course of peer support
4. Begin participation with Berks County’s Forensic Mental Health Case Management Program
5. Begin pre-trial supervision until your admission into the CRRP
While in the MHFHP, John maintained exceptional compliance, ongoing eagerness to stabilize his health, and significant initiation in life goal achievement, behaviors of motivation towards rehabilitation, and insight into his own pathology as affected by TBI. John was able to live in an independent living setting and comply with all re-integrative supports during the one-month admission into the MHFHP.
CRRP Admission and Dismissal of Charges
John completed the one-month re-integrative condition of his unsecured bail. He was then admitted into the CRRP. All of his charges were dismissed at this point and he was not convicted on any of his original charges.
John was admitted and living at the CRRP which is approximately ninety minutes away from his residence. He was in the CRRP for about four months where the focus is on long term cognitive rehabilitation treatment for early onset TBI individuals. John is now connected to a team of professionals as he lives independently in a CRRP apartment. To date, John has displayed exceptional improvement during his rehabilitation process. He no longer carries any psychiatric diagnoses and his only active medical diagnosis is Early Onset TBI.
John’s immediate goals for the future are to re-enroll into college, continue his road to TBI understanding, independent living, and becoming an advocate for TBI awareness among our youth.
Case Example II: Jane Doe Mental Health Forensic Intercept Point 2 (A2)
Mental Health Forensic Diversion Intercept Narrative for Jane Doe
Jane Doe was referred to the forensic diversion program by a mental health case management provider who asked for a diversion assessment for her client. The Blended Case Manager (BCM) reported that Jane has an upcoming trial for theft of $55,000.00 from a non-profit social club where she volunteered to manage the financial records and related charges. Jane was referred to us at pre-trial intercept point of diversionary intervention.
Jane’s diversion narrative consists of several layers of mental health, criminology, and pathological behaviors that exacerbated her ability to formulate healthy and rational decisions in the 16 months leading up to her arrest. Her case manager reported that Jane was employed for numerous years as a financial auditor for a private business, but that she consistently struggled with her mental health stabilization, thus the need for case management services.
Her BCM continued to discuss that Jane is morbidly obese, lived in isolation, had poor physical mobility, few social contacts, and a chronic feeling of suicidality. It was reported that Jane was active in treatment; however, it was difficult for her to manage consistent appointment attendance and commitments due to her limitation with transportation and the distance her current residence is from nearby towns and cities.
Jane’s case presentation for referral at the pre-trial intercept point was atypical. Generally, the forensic diversion program does not address theft charges in this range as a precautionary factor in dealing with monetary bail conditions. However, it was in the best interest of Jane that the diversion specialist consulted with the assistant district attorney (ADA) assigned to the case. Knowing the ADA is an advocate for mental health criminal justice support, a diversionary plan that offers support and other options was presented. This consultation was before the diversion specialist met Jane, but based on the reliability of the BCM’s relationship with her and the overall extent of her crime, there was a need for an immediate consult which was done in an effort to save time and/or rule out any denial of such plan for related crimes. The ADA reported that Jane is facing numerous federal and state charges. He stated the federal charges would most likely be dismissed at the pre-trial level, but Jane would still face serious charges with the likelihood of extensive jail time. The Diversion Specialist offered consideration to assess Jane and determine an underlying mental health pathology that could rule out any motive to commit such crimes. Based on Jane’s referral presentation, Jane’s quality of life was presented to help the court make conclusions as to any level imminent risk she would present to the community. The ADA agreed to hold the charges for continuance of one month until a full assessment could be completed and recommendations made to the court.
Initial Referral Our Program
The Diversion Specialist met with Jane two days after receiving the initial referral from her BCM. Jane, her BCM, and a diversional specialist met at Jane’s home for approximately three hours. This was to conduct a MHFDA in order to rule out motive and to support any exacerbated mental health pathology as the driver to her crime.
Mental Health Forensic Diversion Narrative
Jane presents as morbidly obese and physical limited in mobility. She required a walker to help move throughout her apartment. Jane appeared moderately hygienic and there were some concerns with her ability to maintain herself and her home. However, this could be due to her obesity and limited mobility.
Jane reported that she has been in mental health treatment her whole life and added that her life has been marred with significant trauma, abuse, neglect, and minimal supportive networks. Jane reported that as she aged, she did develop more supportive friendships. She continued to report that she has always held employment and believes in working hard to be a responsible citizen. Jane reported only a high school education but that she has developed a skilled set in tax preparation and financial records administration type services.
Brief Real Time Psycho-Forensic Assessment and Evaluation
Jane reported the last three years have been very difficult as her weight increased and she became less mobile. She mentioned the difficulty she had in getting to work regularly and subsequently earning an income relative to her daily living needs. It was also around this time that she started playing video gambling games on the internet. Jane reported these games cost money and she started paying to play. It was also at this time that she volunteered at a local non-profit social hall to help manage the finances. Jane reported the past three years she became addicted to video gambling and subsequently funded her addiction by stealing funds from the social hall. She was able to detail each occurrence of theft, the amount of each theft, and what the stolen funds covered in way of her addiction and daily living needs.
Upon presentation, Jane appeared labile, moderately depressed and with mild anxiety type features in mood and affect. She was open to discussion but guarded with personal and historic questioning. Jane displayed concerns with a poor lifestyle of wellness and with moderate concerns of hygiene. She reported, “I have not cared about my weight and health for a long time. I have been so depressed and angered about my trauma and terrible family supports. I just let myself go”. She does not present any psychotic features and she is orientated to person, place, and time. She is an intelligent, elderly woman in her 60’s that does display quality of insight and rationalization. There were no cognitive or thought disorder concerns. Jane reported several areas of social relationship isolation and an inability to form adequate emotional relationships. She reported, “I have lost complete trust in any one person to care and love. I have no one, and everyone in my life has abandoned me or taking advantage of me. I was abused atonally, bullied often, and ignored by kids as a child and later by adults. So, I just don’t know how to form good friendships that I can trust.” Jane presented as a survivor of abuse to some form on an emotional level. Her overall personality is like a depressive type personality disorder. When asked about the gambling abuse and theft of the funds, she stated, “I am addicted to those games, it’s the only thing that makes me feel something. I feel in control. I started stealing the money knowing I would get caught. But I didn’t care. I didn’t want to feel depressed anymore, those video games and gambling helped numb my depression and my abusive past.”
At the conclusion of the assessment, it appeared that Jane was living with some form of a personality disorder, possibly a depressive type. This personality disorder most likely developed as a behavior need to survivor and cope. Her overt behaviors say addiction; however, when the layers of her pathology are removed, it was concluded that Jane is in emotional despair.
Based on the assessment, it was recommended that Jane be considered for acceptance into the diversion program. Jane would not benefit from being in prison, a diversion from a prison sentence would serve to help Jane become a contributor to society by paying restitution and improving her overall quality of life.
Mental Health Forensic Diversion Plan
Recommendations were made to the ADA, Jane’s legal defense, the victims, and the presiding judge for Jane’s case. Based on Jane’s overall level of poor health, her underlying features of marked abuse and neglect, her willingness to comply with treatment, her ability to pay full restitution, and the conclusion that her motive was not to steal money, but rather to not feel her depressive pathology. Jane needed to cope with her pathology, she endeavored to a place of addiction as means to feel. Understanding the crime itself is significant, her behavior in the crime would not serve to help Jane return to society after a lengthy prison sentence.
Jane’s case presented with numerous
variables, of which diversion has not historically offered to support in the
past. It was clear Jane did not have a criminal motive, she was not an imminent
risk to society, and she was genuinely willing to offer full restitution. Jane
was facing numerous charges, of which carry a minimum sentence of 6-8 years in
state prison. I presented the following recommendation for Jane’s diversion
from a conviction and sentencing to state prison:
1. Agree and comply with all recommendations at the point of agreed continuance of your charges to unsecured bail.
2. Agree and comply with all conditions upon your admission into the Berks County Mental Health Forensic Transitional Housing Program offered through our program.
3. Agree and comply with all recommendations upon admittance into our county’s Intense Outpatient Program (IOP) and Addiction Treatment Group.
4. Agree and comply with all recommendations upon your admission into our county’s mental health treatment court program.
5. Agree to pay 75% of the restitution with in the first year and the remaining 25% of the restriction with in the second year.
6. Agree and comply with all treatment recommendations upon admission into our Wellness/Lifestyle Program.
7. Agree and comply with all psychiatric medication management recommendations upon admission into our Psychiatric Outpatient Program.
8. Agree and comply with all recommendations by your step-down provider upon completion of the IOP.
9. Agree and comply with all services offered through SAM, Inc. upon completion of the intake.
10. Agree and comply with all recommendations provided by your peer specialist.
11. Agree and comply with all recommendations made by the Mental Health Forensic Diversion Program.
12. Agree and comply with all recommendations upon admission into our Job Readiness Program.
13. Agree and comply with all treatment recommendations made by your entire support team.
The victims, Jane’s legal defense, ADA, and the presiding judge all agreed to support Jane with the recommended plan. Jane was placed on unsecured bail and ordered to comply with the above plan. She also had status hearing checks in court every two months for the next year. If she maintains her compliance for the next year, she will only be convicted of a much lesser charge and never set foot into a prison.
Diversion Outcome
Jane was able to comply with the entire plan for one year and was able pay full restitution back to the victim over the course of 18 months. She gained meaningful employment and started living a life of wellness, independence, and recovery. Presently, Jane is living independently and recently completed her last cycle of mental health treatment court. She has only received one conviction of a summary offense.
Jane’s case offered a moment to really pay attention to what drives overt criminal behavior—often taking time to listen, the person can be understood, and services are not fixated on the crime. When the layers of a person’s criminal actions are peeled away, and time is taken to learn what drives such behavior, then more help can be offered as opposed to incarceration. Jane’s case was a complete stretch to support based on her theft and its amount. This is an excellent example of the judicial system working to help and not incarcerate.
Conclusion
Throughout the past several years, the forensic diversion program has offered individuals with mental illness and criminal charges an opportunity to engage in treatment to address their mental health concerns and/or other concerns that directly affect their behavior and interactions with others. The case studies presented above are just two examples of this program’s success.
Our success is a direct reflection of the collaboration of our county’s stakeholders shared with the development of our program. The impact of this collaboration has born significant fruit in continuity of care. The continuity to foster support for this population among all stakeholders, public office, law enforcement departments, and treatment providers is a direct reflection of the regard each office has for the mental health population.
To continue our program’s goals of collaboration and continuity within the mental health forensics population, our team conducts law enforcement trainings, presents at national conferences, provides community education, and continues to engage our citizens about the desensitization of the mental health population.
References
- Council of State Governments Justice Center. The Stepping Up Initiative: The Problem. 2020. https://stepuptogether.org/the-problem. Accessed March 16, 2020.
- Council of State Governments Justice Center. Improving outcomes for people with mental illnesses involved in New York City’s criminal court and corrections system. 2020. http://csgjusticecenter.org. Accessed March 16, 2020.
- James D.J, Glaze LE. Mental health problems of prison and jail inmates. Bureau of Justice Statistics. 2006. https://www.bjs.gov/content/pub/pdf/mhppji.pdf. Accessed March 16, 2020.
- Fisher WH, Roy-Bujnowski KM, Grudzinskas AJ, Clayfield JC, Banks SM, Wolff N.
Patterns and prevalence of arrest in a statewide cohort of mental health care
consumers. Psychiatric Services. 2006;57(11):1623-1628.
- SAMHSA (no details)
- Christie A, Clark C, Frei A, Ryerson S. Challenges of diverting veterans to trauma-informed care: The heterogeneity of intercept 2. Criminal Justice & Behavior, 2012, 39:461-474.
Appendix 1
Tracking Statistics: Programs Inception through March 2020
Referral
Source Tracking Statistics:
· Total # of Referrals: 1112
· Referrals from Police: 398
· Referrals from Courts: 376
· Referrals from Jails/Prison: 244
· Referrals from Family, Agencies, Hospitals, Others: 94
Diversions Tracking Statistics:
· Total # of Diversions from Mental Health Forensic Intercept Points: 626
· Total # of Diversions at Intercept 0 (A2): 326
· Total # of Diversions at Intercept 1 (A2): 98
· Total # of Diversions at Intercept 2 (A3): 84
· Total # of Diversions at Intercept 3 (Detainment/Jail/State Prison): 118
· Total # of Diversion Referrals (Criteria not met): 486
Total Charges & Convictions Diverted from:
· Total Charges (summaries, misdemeanors, felonies): 1408
· Total Summaries Diverted or Dismissed: 821
· Total Misdemeanors Diverted or Dismissed: 433
· Total Felonies Diverted or Dismissed: 154
Total Re-Arrest and/Recidivism
· Total New Arrests: 33
· Total Arrests while in the diversion program: 17
· Total Arrests after completion of diversion program: 16
Appendix 2
Berks County Mental Health Forensics Program
Definition of Terminology Commonly used in our Program
1. Brief Real Time Psycho-Forensic Diversion Evaluation and Assessment: Our programs clinical interview that concludes a contact referrals likelihood to present imminent risk based on mental health diagnosis and symptoms. Based on the contacts presentation during our programs interview we will determine if the contacts current behavior is based on exacerbation of mental health pathology or if there is a criminal motive for which contact is presenting.
2. Jail Based Diversion Planning: Based on our programs assessment and evaluation we conclude the contact would be better served in a treatment program specified to their current mental health pathology, thus diverting them from jail. Our program then prepares recommendations to the court for the court’s ruling on diverting the person from jail and into a specified treatment program.
3. Mental Health Forensic Diversion Contact: Any person who is referred to the program at any of the four intercepts points of diversion.
4. Mental Health Forensic Intercept Point 0: Any diversion referral provided through Family, Supports, and/or police prior to an arrest.
5. Mental Health Forensic Intercept Point 1: Any diversion referral provided at an arraignment or arrest point of intervention.
6. Mental Health Forensic Intercept Point 2: Any diversion referral provided at the pretrial, sentencing and/or conviction point of contact.
7. Mental Health Forensic Intercept Point 3: Any diversion that occurs at the detainment, local jail, state prison and federal incarceration point.
8. Mental Health Forensic Diversion: Any effort made to support an individual living with a mental health disorder and their transitioning from one of the four intercept point and into treatment-based program, all the while removing the likelihood on continued criminal justice involvement
9. Mental Health Forensic Intercept Narrative: The referral sources initial observation, information, and/or concerns for the referral at the initial point of contact
10. Mental Health Forensic Presenting Narrative: The Mental Health Forensic Diversion Specialist initial discussion of the contacts global and historical personal information as relevant to their involvement at the presenting intercept point.
11. Unsecured Bail Diversion Plan: Based on our programs evaluation and assessment we recommend the person be placed on a bail plan which rules the person is to comply with our program’s recommendations for an unspecified period of time. The unsecured bail plan carries no monetary responsibility to the person, but conditions of compliance.
Biography
Jillian Gosselin, MSW, LSW, CPSS, is a Diversion Specialist and Forensic Blended Case Management Supervisor at Service Access & Management, Inc., Berks County, Pennsylvania. She has worked to further develop the Forensic Mental Health Diversion Program, with Mr. Brandon Sands, as well as develop and expand case management services specifically for the forensic mental health population. Ms. Gosselin graduated from Albright College with a Bachelor of Arts Degree in Psychology and from Marywood University with a Master’s Degree in Social Work. Over the past 17 years, Ms. Gosselin has presented at National and International Conferences in various topics including mental health, drug and alcohol, sex workers, prevention of high-risk behaviors among youth, and HIV prevention.
In addition to her work in the behavioral health field, she continues to work as an independent consultant, writing grant proposals, analyzing data, and working with a highly qualified evaluation team for federally funded substance abuse grant programs focusing on at-risk populations. Ms. Gosselin also works as a Peer Reviewer for SAMHSA grant applications. In previous years, she has worked as an Adjunct Professor of Psychology at Albright College in Reading, Pennsylvania.
Ms. Gosselin resides in West Reading, Pennsylvania with her husband, Mark, and 10-year-old daughter, Sara. In her free time, she enjoys spending time with her family and playing soccer in a competitive women’s league.
Contact Information:
Jillian Gosselin, MSW, LSW, CPSS
Diversion Specialist and Forensic Blended Case Management Supervisor at Service Access & Management, Inc
(484) 987-5321
Biography
Brandon Sands, LPC, NCC, CABA, CPSS has assisted in the development of the Berks County (Pennsylvania) Mental Health Forensic Diversion Program. Over the past 10 years, he has implemented specific psycho-forensic parameters to assist in the diagnosis, treatment and reintegration of the Forensic Mental Health Population. He speaks nationally on various topics regarding the training, treatment, education, development and psychopathy of the Mental Health Forensic population. Mr. Sands, along with Ms. Gosselin, have developed specified restoration and reintegration services, guidelines, programs and initiative to assist with national awareness and training for those providing any level services and support for this population.
Along with his work in the psycho-forensics field, Mr. Sands is also an Adjunct Professor of Psychology for the past 17 years at Alvernia University. He is partner in a private practice that serves five counties in Pennsylvania. In private practice, his treatment focus is primarily with clinical, testing, sports, anxiety, and behavioral-related areas of practice. Mr. Sands is a Licensed Certified Applied Behavioral Analyst that provides various testing, diagnosis, and treatment services for the Intellectually Disabled populations.
Contact Information:
Brandon Sands, LPC, NCC, CABA, CPSS
610-763-8537
Basands1@icloud.com




